Achieving a 15% reduction in body weight can enable nearly 90% of individuals diagnosed with type 2 diabetes for under four years to enter remission.
At present, over half a billion adults worldwide are living with diabetes, and projections indicate a roughly 50% rise in prevalence within the next generation. While numerous resources highlight optimal dietary approaches for managing diabetes, an intriguing alternative involves forgoing food intake altogether through fasting.
More than 100 years ago, medical literature described fasting as a potential cure for diabetes, capable of rapidly stopping disease progression and eradicating symptoms within mere days or weeks. However, prolonged starvation inevitably leads to severe health consequences, including the total depletion of bodily reserves. The challenge lies in the fact that weight lost during fasting often rebounds quickly upon resuming previous eating patterns that contributed to the weight gain initially. Could fasting serve as a catalyst to initiate sustainable healthier eating habits? Scientific evidence provides valuable insights into this question.
Type 2 diabetes has historically been viewed as a condition stemming from excess, primarily affecting those with sedentary lifestyles and abundant resources. It was once associated with “the idle rich,” individuals whose daily lives lacked rigorous physical activity and whose finances allowed overconsumption beyond bodily needs. Given its preventable nature, diabetes may also prove treatable through targeted interventions. If overeating contributes to mortality from this disease, could deliberate undereating offer a path to recovery? This concept echoes an ancient Ayurvedic recommendation from approximately 2,000 years ago, which advised those with limited resources suffering from diabetes to adopt an austere lifestyle: living simply like a hermit, engaging in extensive physical labor such as walking vast distances or digging ponds, or even subsisting on minimal, unconventional fare.
This historical perspective calls to mind the Rollo diet introduced in 1797 specifically for diabetes management. It consisted primarily of rancid meats, supplemented by emetic drugs akin to ipecac to provoke intense nausea and vomiting. Such interventions temporarily alleviated diabetes symptoms by drastically curbing food consumption. The regimen featured unappetizing elements like congealed blood for midday meals and putrid meat for evenings, effectively reducing intake through revulsion.
Comparable improvements occurred among diabetic patients during the Paris siege in the Franco-Prussian War, prompting the guideline to consume as little food as feasible, or “mangez le moins possible.” This approach evolved into the formalized Allen starvation therapy, hailed as the most significant breakthrough in diabetes care before insulin’s advent, marking what became known as the Allen Era.
Dr. Allen observed clinical accounts where advanced diabetes resolved spontaneously amid wasting illnesses like tuberculosis or cancer. Inspired, he tested controlled underfeeding and discovered that even in grave cases, urinary sugar could be eliminated within ten days. Maintaining this clearance proved more challenging once normal eating resumed. His protocol emphasized two key strategies: maintaining patients in an underweight state and minimizing dietary fat. Individuals with severe diabetes might remain asymptomatic for extended periods, yet reintroducing fats like butter or olive oil could swiftly reignite symptoms.
As previously discussed, type 2 diabetes fundamentally arises from fat toxicity. Research demonstrates that infusing fats intravenously leads to rapid fat accumulation in muscle cells, observable via advanced MRI technology, alongside diminished insulin sensitivity within hours. A three-day high-fat diet yields similar muscle fat buildup and insulin resistance. Strikingly, this effect can manifest after just one day or even a single high-fat meal, elevating insulin resistance within six hours. Acute fat consumption promptly impairs insulin responsiveness. This matters because muscle insulin resistance, amid caloric surplus, promotes hepatic fat deposition, progressing to pancreatic fat accumulation and culminating in overt diabetes. Contemporary understanding frames type 2 diabetes as excessive fat storage in the liver and pancreas, a reversible state for at least a decade in most cases.
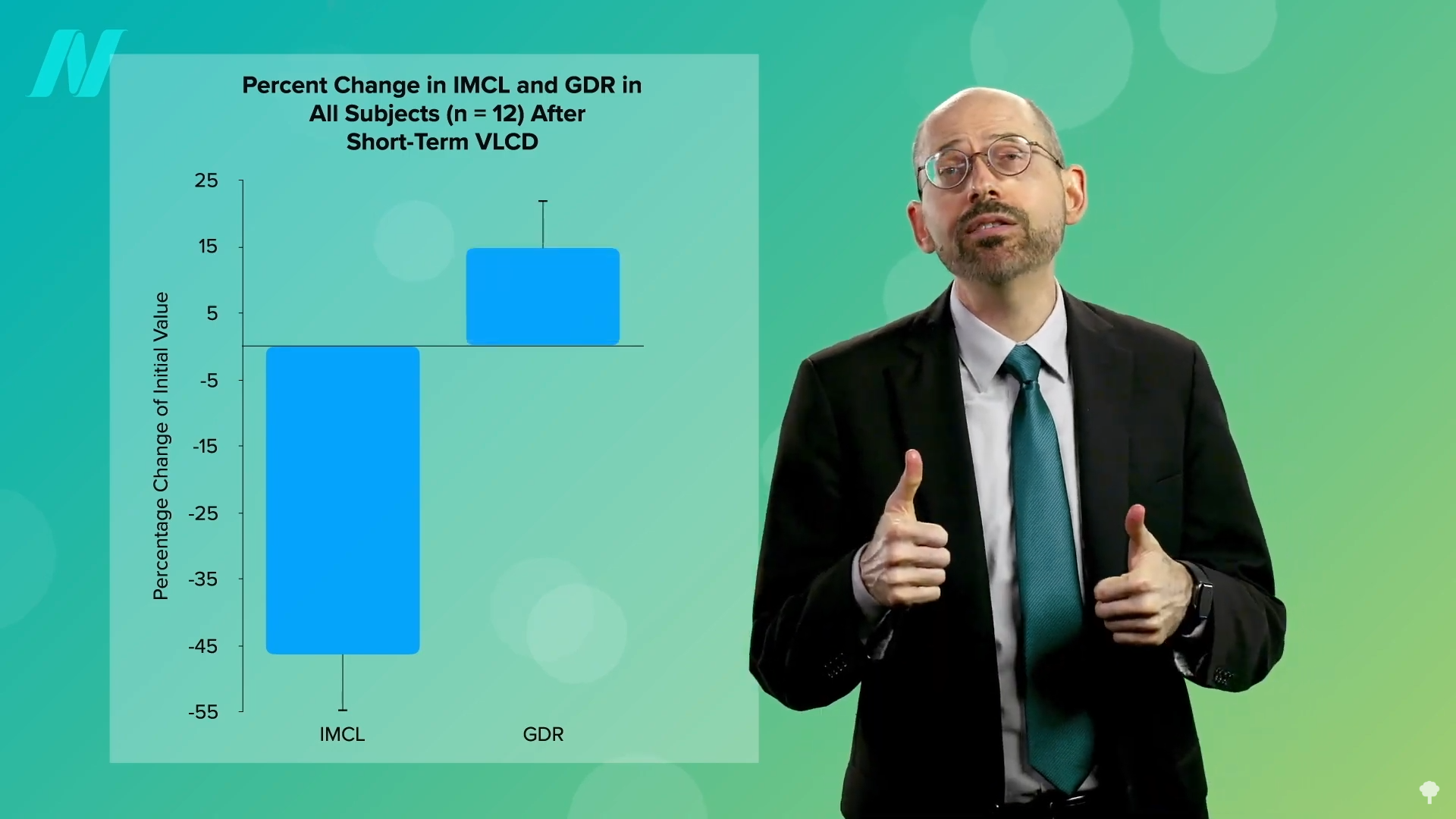
Implementing an extremely low-calorie regimen, such as 700 calories daily, mobilizes fat from muscle cells, enhancing insulin sensitivity correspondingly, as illustrated in studies.
Liver fat levels subsequently plummet significantly, and with sustained adherence, pancreatic fat diminishes too. Early intervention allows reversal of type 2 diabetes, fostering stable blood glucose on a nourishing diet.
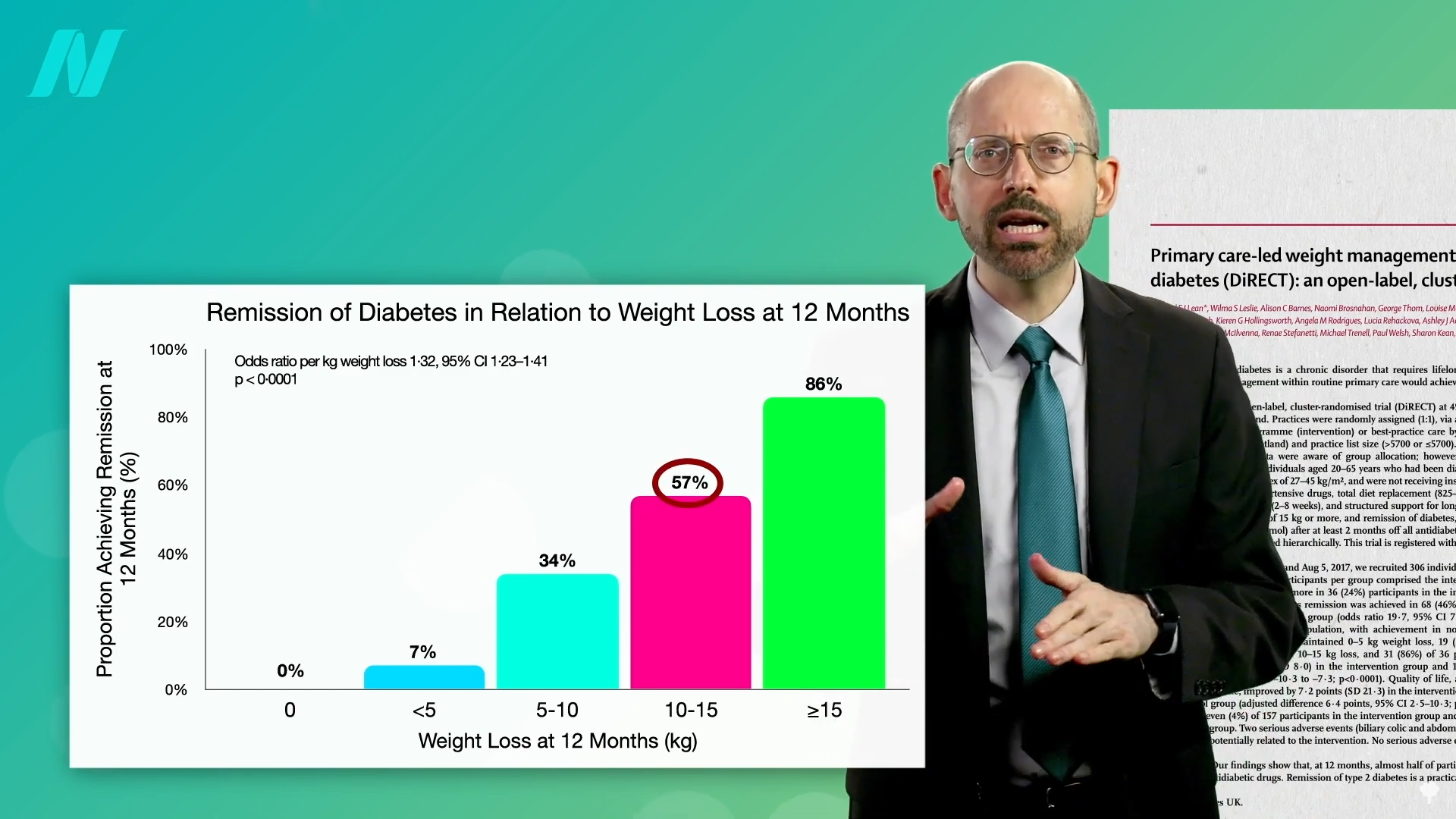
Shedding 15% of body weight enables nearly 90% of those with type 2 diabetes duration under four years to attain non-diabetic glucose control, compared to about 50% for those enduring over eight years. These outcomes surpass bariatric surgery results, where greater weight loss yielded only 62% and 26% remission rates, respectively. Dietary changes via everyday utensils outperform surgical interventions. Indeed, patients averaging three years post-diagnosis can reverse their condition after dropping around 30 pounds.
Physician-monitored water-only fasting can achieve comparable weight loss and remission, but sustaining the reduced weight remains essential. Research confirms unequivocally that weight regain parallels diabetes recurrence.
Reflecting on history, the initial excitement over insulin’s 1921 discovery as “medicine’s greatest miracle” tempered as it proved insufficient alone for type 1 diabetes survival but inadequate to avert type 2 complications like vision loss, renal failure, strokes, and limb amputations. Pioneering diabetologist Elliott Joslin advocated reinstating pre-insulin emphasis on disciplined diet and exercise as core to effective management.
Key Takeaways
- Type 2 diabetes frequently proves reversible, particularly soon after onset. A 15% body weight reduction can induce remission in nearly 90% of cases under four years, with viable prospects even for longer durations at reduced rates.
- Excess fat in the liver and pancreas underlies type 2 diabetes by disrupting insulin action. Brief high-fat exposures suffice to heighten insulin resistance.
- Though fasting may initiate remission, preserving weight loss proves paramount. Enduring dietary and exercise adherence outperforms bariatric procedures for sustained reversal.









