For more than 2,400 years, since the era of Hippocrates, the practice of fasting has been recommended as a potential remedy for both acute and chronic illnesses. This approach stems from the common observation that individuals who fall ill often experience a natural reduction in their desire to eat.
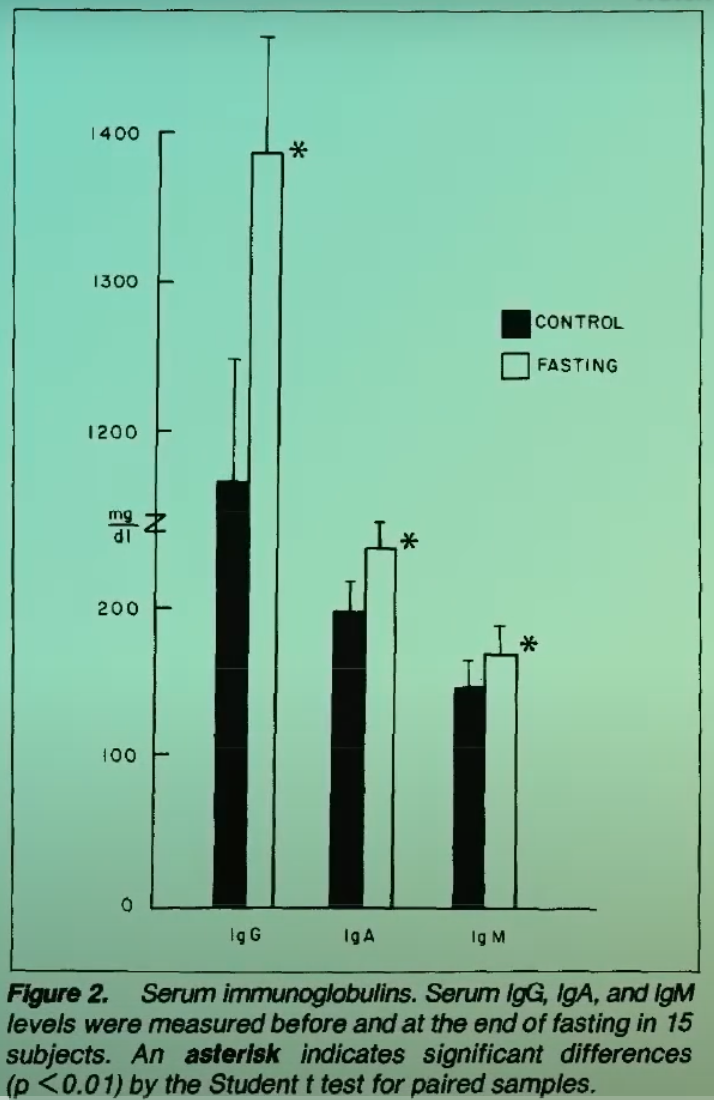
In addition to fever, a decrease in food intake represents one of the most prevalent indicators of infection. While it is sometimes viewed as an unwelcome symptom of illness, this response actually serves as an intentional and advantageous protective strategy. As explored in related discussions on fasting and cancer-related weight loss, prolonged nutritional deficiency can weaken our immune responses over time. However, evidence indicates that temporarily reducing calorie consumption in the short term can actually strengthen immune capabilities.
Scientific investigations have demonstrated that blood drawn from mice subjected to starvation exhibited nearly eight times greater effectiveness in eliminating invading bacteria within a laboratory dish. This remarkable enhancement significantly amplified the pathogen-destroying power of their white blood cells. Researchers have extended these findings to humans and are now examining implications for cancer treatment.
Does Fasting Boost Natural Killer Cells Against Cancer?
In a study where participants adhered to a severely restricted diet of just 80 calories per day for two weeks, their white blood cells displayed a notable improvement in their capacity to destroy bacteria and produce antibodies. Furthermore, the activity of their natural killer cells rose by an average of 24 percent. This finding holds particular significance since natural killer cells play a crucial role not only in combating infections but also in targeting and eliminating cancer cells. In fact, scientists assessed natural killer cell function by observing their interactions with K562 cells, which are derived from human leukemia.
Fasting is believed to enhance the body’s anticancer immunosurveillance mechanisms, or, in more vivid terms, it awakens the immune system’s hunger for destroying malignant cells. Despite these promising insights, fasting is not more widely adopted in cancer therapy primarily because much of conventional cancer management focuses on maintaining patient weight to combat the debilitating wasting condition known as cachexia.
Understanding the Roots of Cancer Cachexia
Historically, fasting has been overlooked as a viable option in cancer care due to the emphasis in palliative treatments on preventing weight loss and addressing cachexia, a severe wasting syndrome that contributes to mortality in numerous cancer cases.
Cancerous tumors are highly demanding, growing rapidly and requiring substantial amounts of energy and proteins. To sustain themselves, they metabolically reprogram the host’s body, prompting the breakdown of tissues to supply the tumors’ needs. This process involves widespread inflammation triggered by the malignancy. Beyond mere appetite suppression, the weight loss in cancer cachexia differs fundamentally from that of simple starvation because it cannot be reversed by refeeding alone.
Efforts to intervene nutritionally and reverse cachexia often prove unsuccessful. The most effective strategy remains treating the underlying cancer to eliminate its cause. Intriguingly, compelling patients to consume extra nutrition might inadvertently benefit the tumor. Similar to how a fetus prioritizes nutrients during pregnancy, even at the mother’s detriment, tumors may claim first access to available resources. This suggests that the appetite loss accompanying cancer could be an adaptive, protective mechanism evolved by the body.
Evaluating Chemotherapy’s Limitations
Over the last half-century, chemotherapy has emerged as a cornerstone therapy for diverse cancers. Its primary mechanism involves damaging cancer cell DNA through the generation of free radicals. Initially thought to selectively target tumors, it became clear that healthy cells also suffer significant harm, resulting in dose-limiting toxicities such as bone marrow suppression, immune compromise, exhaustion, nausea, digestive issues, and occasionally fatal outcomes.
Survivors of chemotherapy face the added risk of secondary cancers arising from DNA damage in normal cells. Protective agents have been tested to mitigate these side effects, enabling higher chemotherapy doses, but they fail to extend survival rates—possibly because they inadvertently shield cancer cells as well. An alternative approach involves using fasting to safeguard healthy cells during treatment.
The Synergy of Fasting and Chemotherapy
The protective and therapeutic potential of fasting in cancer management remains underappreciated by many. Implementing short-term fasting before and right after chemotherapy sessions could lessen adverse effects while heightening cancer cells’ vulnerability to the drugs. This dual action presents a compelling advancement.
When deprived of nutrients, normal cells shift into a survival mode focused on maintenance and repair. In contrast, tumor cells, driven by oncogenic mutations, cannot decelerate their rampant proliferation and thus remain susceptible during nutrient scarcity. This metabolic inflexibility serves as a critical vulnerability for various cancer types.
These contrasting reactions to fasting between healthy and malignant cells result in chemotherapy inflicting greater DNA damage and triggering more cell death in tumors, while sparing normal tissues. Consequently, brief fasting periods may shield the body from chemotherapy’s toxicity and sensitize tumors—though this remains a hypothesis supported by preclinical data.
In animal models, fasting alone proved comparably effective to chemotherapy in curbing tumor growth. Radiation therapy similarly restrained unchecked tumor expansion, with even superior results when paired with intermittent fasting protocols. Notably, fasting by itself matched radiation’s efficacy in these breast cancer mouse studies, sparking optimism for human applications.
Human Trials Testing Fasting with Cancer Therapies
A group of patients with assorted cancer diagnoses chose to fast before chemotherapy infusions and documented their outcomes. They experienced diminished fatigue, debility, and gut-related issues during fasting periods, reporting overall improvements without any instances of vomiting. The modest weight shed over a few days was rapidly regained by most, with no evident negative consequences. Under medical oversight, fasting appears both safe and capable of easing treatment burdens.
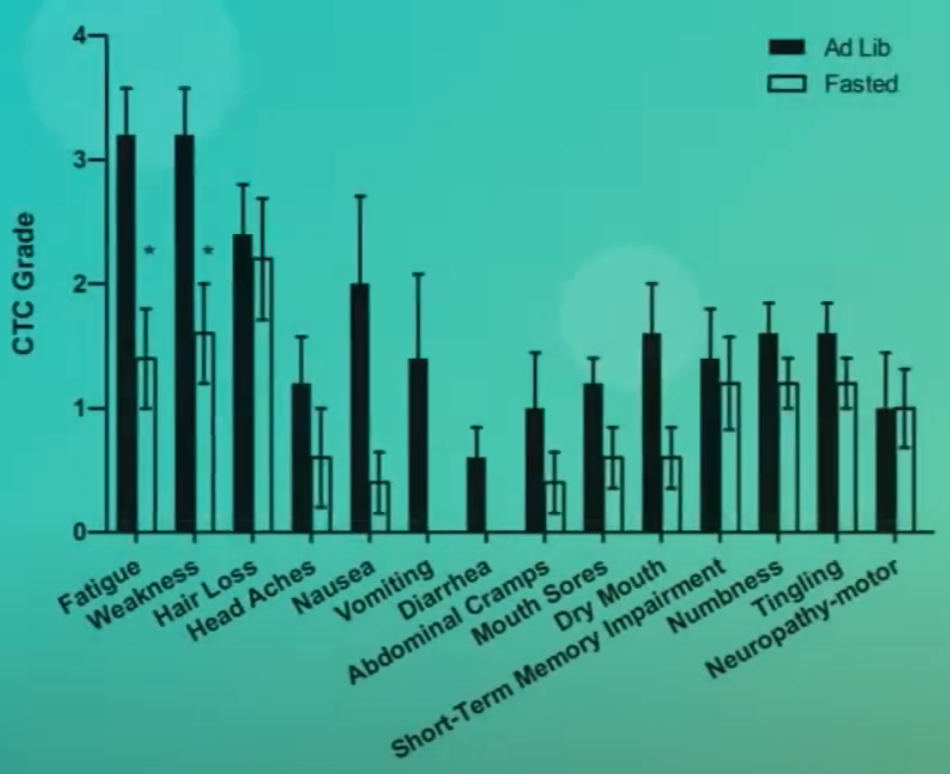
In a controlled trial involving breast and ovarian cancer patients, fasting from 36 hours pre-treatment to 24 hours post-treatment enhanced quality of life and reduced fatigue scores. Contrarily, another trial observed no such gains, though it noted potential reductions in bone marrow toxicity via elevated red blood cell and platelet precursor counts. Disappointingly, white blood cell preservation—the key immune defenders—was not achieved, possibly due to insufficient fasting duration.
A comprehensive analysis of 22 investigations concluded that fasting could mitigate chemotherapy toxicities like organ injury, immune deficits, and treatment-related mortality. It might also hinder tumor advancement, including growth and spread, potentially boosting survival odds. However, the majority involved rodents and canines; human data focused solely on feasibility and symptom relief, leaving tumor control effects unassessed.
Enhancing Chemotherapy Efficacy Through Fasting
Short-term nutrient restriction around chemotherapy addresses a core challenge: eradicating tumors without excessive harm to the patient. Protocols like 48 hours pre-chemo and 24 hours post may curtail toxicities. Yet, fasting’s direct antitumor impacts warrant further scrutiny.
Proponents suggest that alleviating side effects permits escalated dosing, amplifying effectiveness. Cardiotoxicity and nephrotoxicity from common agents constrain their use. Still, evidence linking peak-tolerated doses to superior survival or well-being is inconclusive. For the present, diminishing side effects stands as a worthwhile goal in itself.
Mechanisms Behind Fasting’s Anticancer Effects
Fasting lowers insulin-like growth factor-1 (IGF-1), a hormone that fuels cancer development. This drop facilitates selective safeguarding of healthy cells over cancer cells during nutrient stress and bolsters chemotherapy’s tumor-killing precision while preserving normal tissues.
Diminishing IGF-1 signaling offers twin advantages: shielding healthy organs and impeding tumor growth. It may even avert cancer onset initially. Beyond fasting, which halves IGF-1 after mere days mainly via protein curtailment, moderating protein—especially animal-derived—achieves similar reductions. Protein strongly influences circulating IGF-1, positioning lower intake as a strategy for cancer prevention and longevity.
Protein Reduction as an IGF-1 Lowering Strategy
Comparing plant-based eaters meeting standard protein needs (0.8 grams per kilogram body weight) to lean individuals on typical high-protein American regimens reveals that calorie restriction modestly cuts IGF-1, but plant-centric eating suppresses it more profoundly.
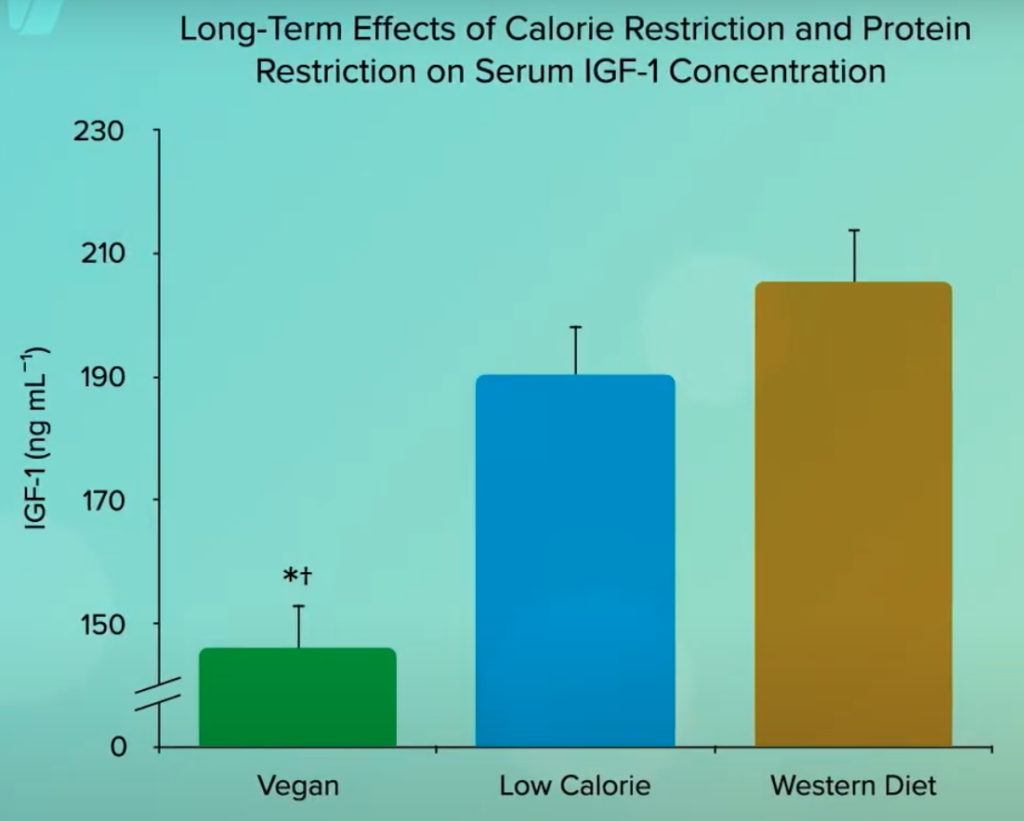
Thus, whole-food plant-based nutrition not only curbs IGF-1 to potentially decelerate aging but also harnesses longevity-associated genes to combat cancer effectively.