Sham surgery studies have demonstrated that several widely performed operations may essentially function as placebos themselves.
Intragastric balloons first gained significant attention back in the 1980s. These devices were designed to be inserted into the stomach and then filled with either air or water, occupying a substantial portion of the stomach’s capacity to promote feelings of fullness. Regrettably, many surgical implements reach the marketplace prior to comprehensive validation of their efficacy and safety profiles, and these balloons followed that troubling pattern.
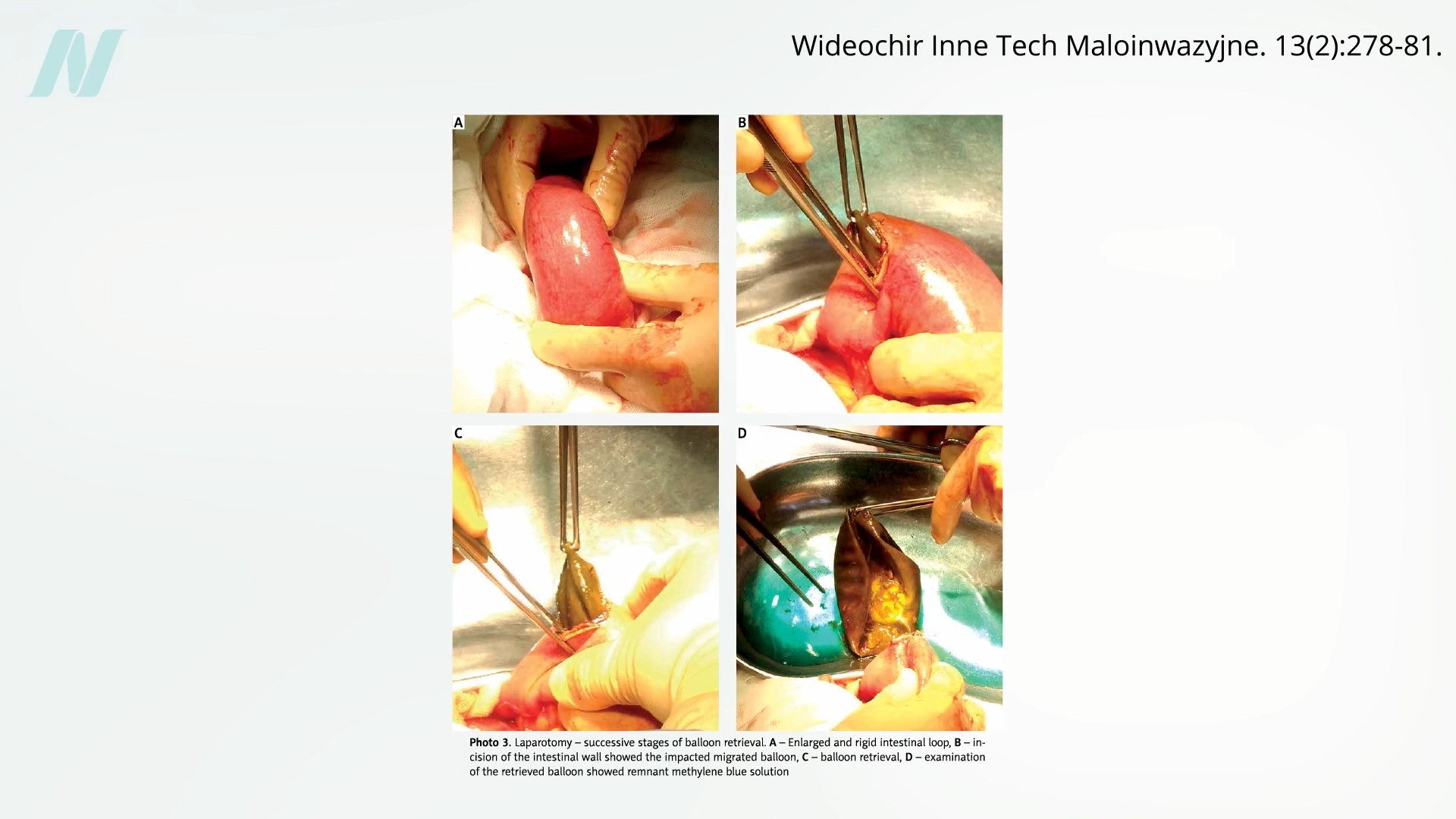
Researchers at the Mayo Clinic conducted an investigation into what was termed the ‘gastric bubble,’ revealing that eight out of every ten such balloons deflated on their own. This spontaneous deflation poses serious hazards, as the devices can migrate into the intestinal tract, leading to potentially life-threatening blockages, as illustrated in the accompanying image captured at the 0:40 mark in the associated video discussion on gastric balloon procedures for weight management.
Prior to deflating, these balloons were found to provoke gastric erosions in approximately half of the patients, resulting in damage to the delicate lining of the stomach. Compounding these issues, comparative analyses indicated that these devices failed to deliver superior weight loss outcomes when pitted against traditional dietary interventions and behavioral modification programs. Consequently, intragastric balloons were eventually withdrawn from commercial availability. However, after a prolonged absence spanning 33 years, the landscape shifted dramatically.
In 2015, the United States Food and Drug Administration began greenlighting a fresh generation of intragastric balloon products, which swiftly led to the implantation of over 5,000 units. This resurgence coincided with the enactment of the Sunshine Act, a legislative measure compelling pharmaceutical firms and manufacturers of surgical and medical devices to publicly report any financial disbursements to healthcare professionals. This transparency initiative cast a revealing spotlight on the various incentives proffered by industry players. While public awareness has grown regarding the intimate financial entanglements between physicians and pharmaceutical giants, fewer individuals appreciate that surgeons similarly receive compensations from device manufacturers for utilizing their products. Data from one year showed that the top 100 physicians accepting such payments pocketed an astonishing $12 million from device companies. Shockingly, when these same professionals authored research publications, only a fraction bothered to acknowledge their glaring conflicts of interest.
One advantage of intragastric balloons compared to many bariatric surgical options lies in their reversibility, allowing for removal without permanent alteration. That said, reversibility does not equate to harmlessness. The FDA has issued multiple safety alerts highlighting grave risks, including fatalities. A pressing question arises: how might a smooth, rounded object precipitate a stomach perforation? The mechanism often involves inducing severe vomiting, which can exert enough force to tear the stomach wall, proving fatal in some instances. Nausea and vomiting emerge as prevalent adverse reactions, impacting the vast majority of patients post-implantation. This ongoing emesis likely underlies reports of severe, potentially lethal nutritional shortfalls following balloon placement.
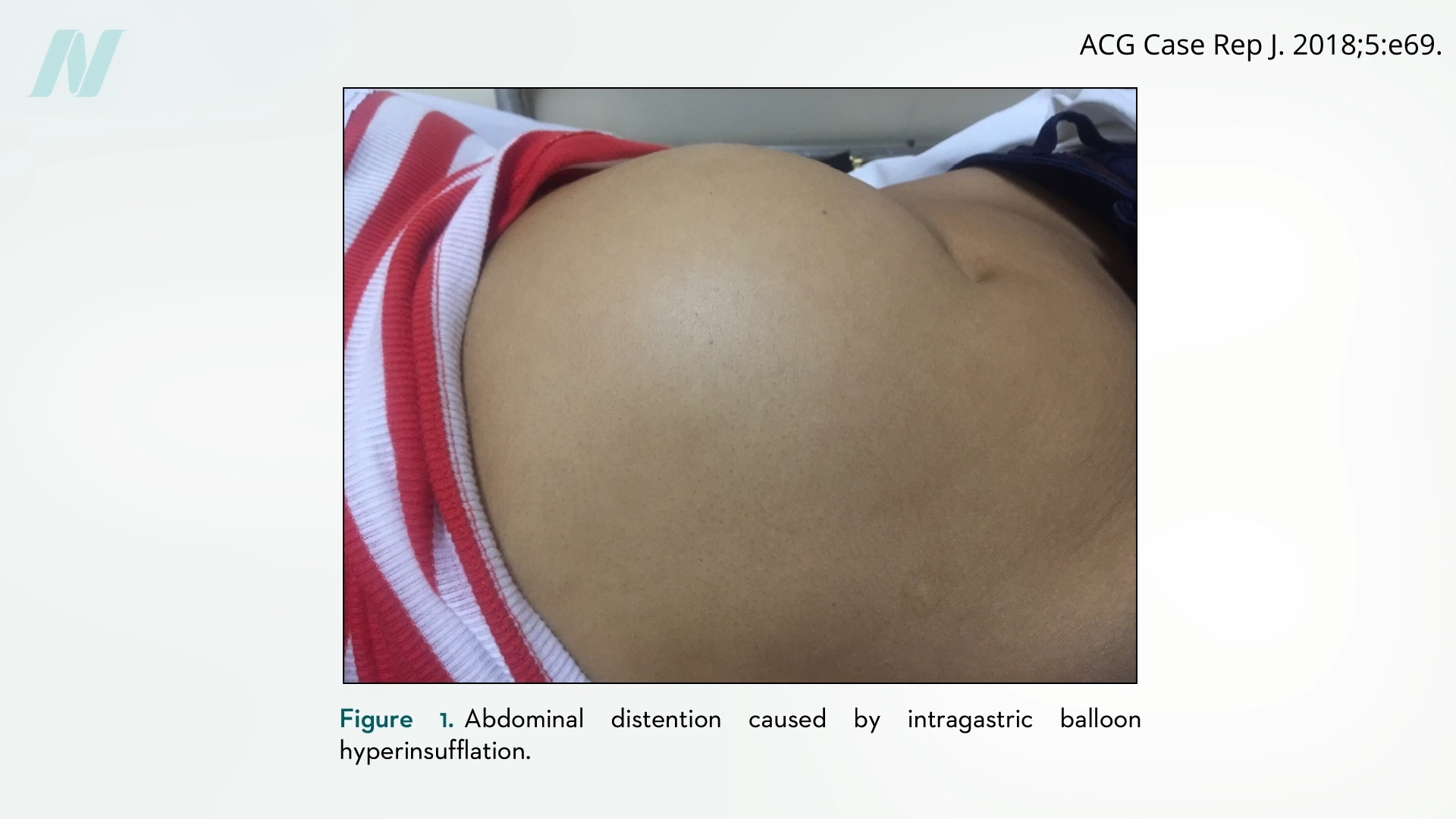
Certain complications, like intestinal blockages, stem directly from balloon deflation. Curiously, other problems arise from unexpected overinflation of the devices, triggering intense pain, vomiting, and bloating of the abdomen, as depicted in the image below from the 2:45 timestamp in the video exploring gastric balloon safety and efficacy.
This peculiar overinflation phenomenon was initially observed in breast implants, with case reports detailing instances like ‘The Phenomenon of the Spontaneously Autoinflating Breast Implant.’ These implants could inexplicably expand, boosting breast volume by more than 50% on average without warning. Experts have described it as an underrecognized and inadequately comprehended occurrence. Notably, breast implants even served as early, unsuccessful prototypes for intragastric balloons in experimental trials.
As with all healthcare choices, evaluating interventions requires a careful balancing of potential risks against anticipated benefits. Trials sponsored by industry have reported substantial weight reductions, yet disentangling the balloon’s isolated contribution proves challenging amid the concurrent implementation of structured diets and lifestyle modifications. In pharmaceutical research, placebo controls using inert pills are straightforward, but replicating a surgical placebo demands ingenuity. Enter sham surgery protocols.
A landmark investigation published in 2002 in The New England Journal of Medicine scrutinized the most frequently performed orthopedic procedure: arthroscopic knee surgery. This intervention, costing billions annually, involves inserting a scope into the knee to excise damaged cartilage in cases of osteoarthritis or injury. But does it truly alleviate symptoms? Participants with knee osteoarthritis were randomly assigned to either genuine surgery or a simulated version, where surgeons made incisions, mimicked the procedure with saline irrigation, but refrained from any actual joint manipulation.
The study ignited fierce controversy. Critics from professional medical bodies decried the ethical implications of subjecting patients to incisions for fictitious operations and questioned the participants’ judgment in consenting. Remarkably, outcomes revealed improvement in both the true surgery group and the sham group alike, as shown in the graph below from the 4:42 point in the video analysis.
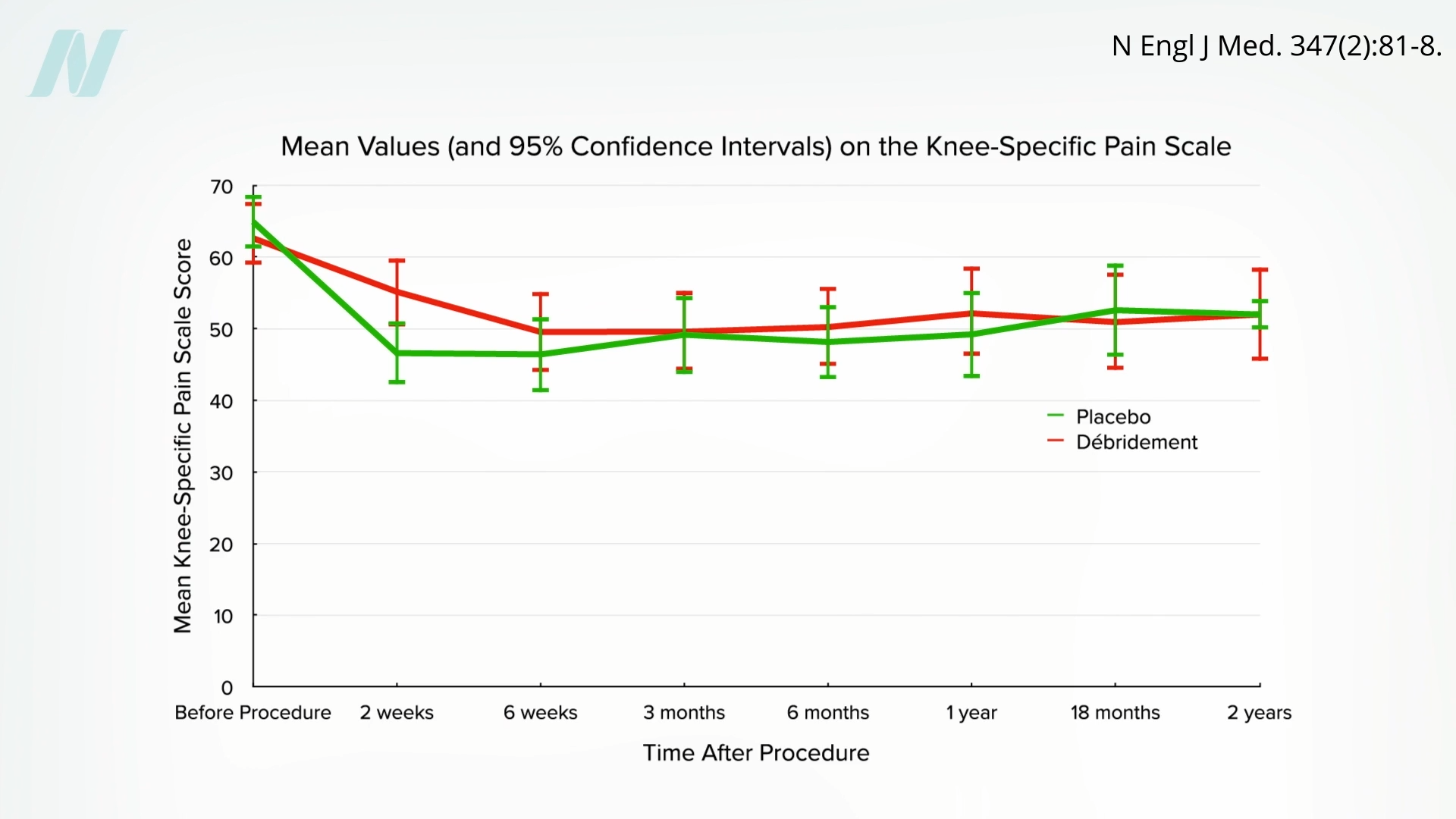
Ultimately, the procedures conferred no measurable therapeutic advantage. Today, similar skepticism surrounds rotator cuff repairs in shoulder surgery, prompting a reevaluation of its validity.
When subjected to rigorous sham-controlled evaluations, both legacy and contemporary intragastric balloons have sometimes demonstrated negligible weight loss advantages. Even in instances of short-term success, benefits often prove fleeting, constrained by regulatory limits permitting only six months of implantation due to escalating deflation perils. Sequential reimplantations have been attempted without yielding sustained weight control. Further sham trials suggest that initial suppressions of appetite and enhancements in satiety may dissipate over time, possibly as physiological adaptation occurs to the device’s presence.
Collectively, sham surgery research underscores a sobering reality: many commonplace operations may owe their perceived success primarily to placebo dynamics. Physicians often position themselves as stewards of scientific rigor, vociferously opposing movements like anti-vaccination rhetoric and decrying societal tendencies to cherry-pick facts for ideological comfort. Yet, confronting evidence that certain enduring surgeries not only lack utility but potentially exacerbate conditions—such as hastening the need for full knee replacements—forces a reckoning with hypocrisy. The medical community, it seems, is not impervious to propagating its own forms of unsubstantiated claims and selective truths.









