Everyday medications, dietary choices, and beverages have the potential to compromise the structural integrity of our intestinal lining, leading to what is known as a leaky gut condition.
Understanding Intestinal Permeability and Its Importance
The concept of intestinal permeability, often referred to as the leakiness of our digestive tract, is emerging as a significant factor in both preventing diseases and developing new therapeutic strategies. Our intestinal barrier, characterized by its numerous microscopic folds and villi, spans an impressive surface area exceeding 4,000 square feet—equivalent to the size of a standard tennis court. Maintaining this vast protective layer demands approximately 40% of the body’s total energy output, underscoring its critical role in overall health.
Scientific research continues to accumulate evidence pointing to the breakdown of this intestinal barrier’s integrity as a key contributor to various health issues, such as celiac disease and inflammatory bowel disease. One innovative method employed by scientists to assess gut permeability involves the use of blue food coloring. In individuals with healthy guts, this dye remains confined within the digestive system. However, in severely ill patients suffering from sepsis—a life-threatening condition where the gut barrier is severely compromised—the dye appears in the bloodstream, signaling significant leakage.
Importantly, developing a leaky gut does not necessitate a critical care admission. Even common over-the-counter pain relievers like aspirin or ibuprofen can trigger this issue relatively easily.
The Impact of Common Painkillers on Gut Health
Clinical studies have demonstrated that consuming just two standard aspirin tablets (each 325 mg) or two extra-strength versions (500 mg each) in a single dose can substantially elevate the permeability of the intestinal lining. These findings indicate that even people in good health should exercise caution with aspirin use, given its capacity to induce dysfunction in the gastrointestinal barrier.
Many turn to buffered aspirin, which combines the medication with antacids to supposedly mitigate stomach irritation. However, investigations reveal no meaningful protective benefit. Both conventional aspirin and buffered varieties, such as Bufferin, result in multiple erosions along the stomach and intestinal walls. Endoscopic examinations conducted on participants revealed widespread erosions and inflammation in the gastrointestinal tract of 90% of those who ingested the recommended doses of either product.
Remarkably, the onset of this damage occurs rapidly, often within mere minutes rather than hours. Research timelines show detrimental effects manifesting in as little as five minutes post-ingestion. In contrast, acetaminophen—marketed as Tylenol in the U.S.—does not typically cause such gastrointestinal harm and may serve as a safer alternative for pain relief, provided there are no pre-existing liver concerns.
Compounding the issue, vitamin C supplements, rather than offering relief, appear to exacerbate the gut leakiness induced by aspirin, according to experimental data.
Painkillers and Their Role in Allergic Reactions
This mechanism may explain why non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen contribute to approximately 25% of cases involving food-induced anaphylaxis. These medications heighten the risk of severe, potentially fatal allergic responses to food by more than tenfold. The presumed pathway involves these drugs enhancing intestinal permeability, permitting minuscule undigested food particles to enter the circulation directly.
Exercise, NSAIDs, and Transient Gut Leakiness
Physical activity, particularly intense exercise, can also play a role. Engaging in strenuous workouts—for example, one hour at 70% of maximum capacity—may redirect substantial blood flow to the muscles, reducing supply to the digestive organs. This shift can inflict temporary injury to the intestines, resulting in mild increases in gut permeability.
Such effects can intensify if athletes consume ibuprofen or other NSAIDs beforehand, a practice that regrettably remains prevalent among sports enthusiasts despite the known risks.
Alcohol’s Contribution to Intestinal Barrier Dysfunction
Alcohol consumption mirrors this pattern, acting as another risk factor for food allergy episodes by similarly promoting gut leakiness. Encouragingly, abstaining from alcohol allows the intestinal lining to repair and regain its protective functions over time.
Dietary Fats and the Promotion of Harmful Gut Bacteria
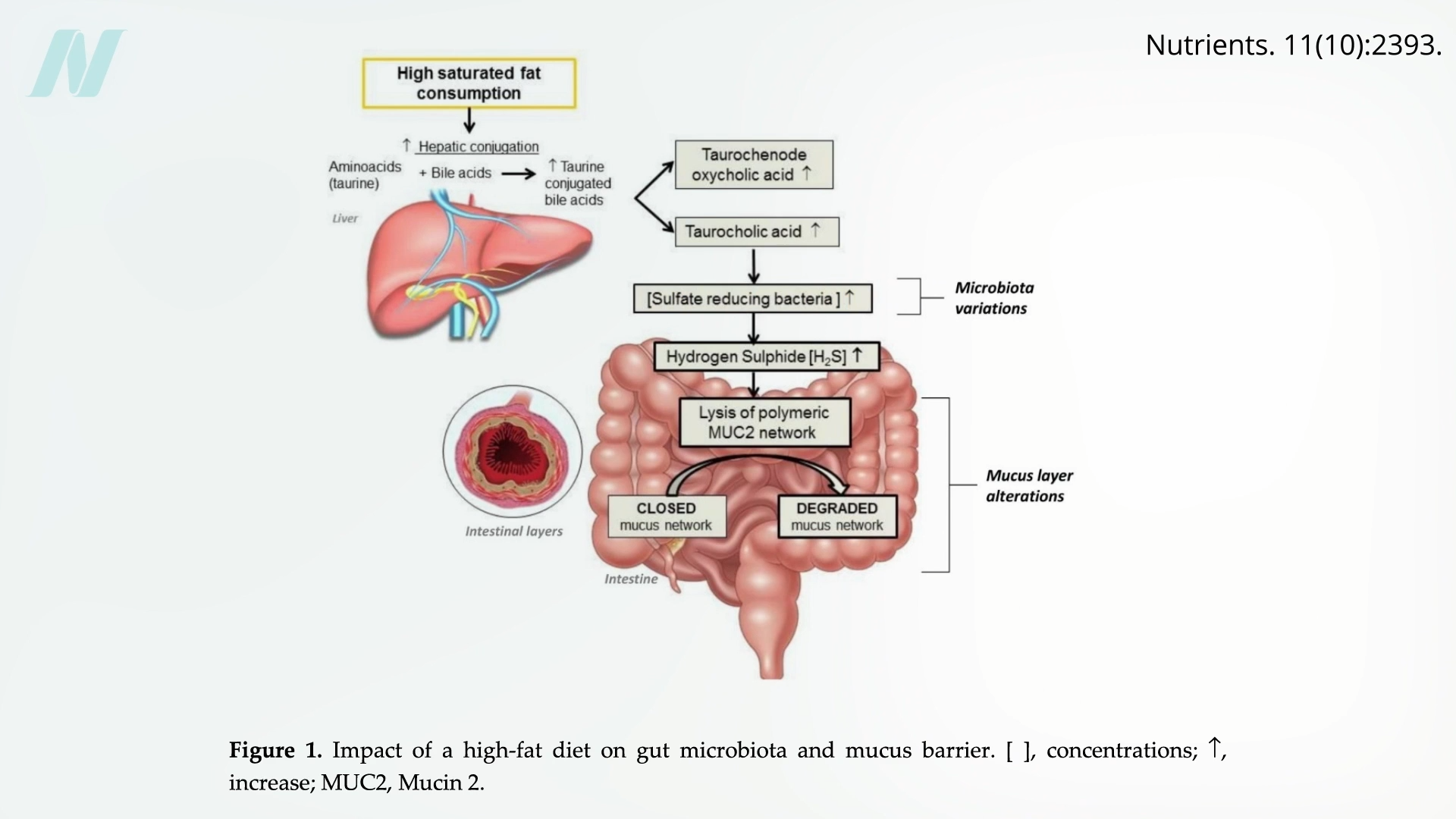
Beyond pharmaceuticals and alcohol, certain elements of our diet can profoundly influence intestinal health. High intake of saturated fats—prevalent in animal products like meat and dairy, as well as processed junk foods—fosters the proliferation of detrimental bacteria. These microbes produce hydrogen sulfide, a foul-smelling gas akin to rotten eggs, which erodes the vital mucus layer shielding the intestinal wall. The accompanying diagram vividly depicts this destructive sequence.
Experts widely acknowledge that diets rich in fats generally impair intestinal wellness by disrupting the barrier system through multiple pathways. While numerous studies in laboratory animals and cell cultures confirm these adverse outcomes, translating these results to humans required direct clinical evidence.
Human Studies on High-Fat Diets and Gut Health
The global surge in obesity and cardiometabolic conditions parallels the shift from traditional low-fat eating patterns to high-fat Western-style diets. Disruptions in the beneficial gut microbiome correlate strongly with elevated risks for these disorders. Animal models illustrate how high-fat feeding disrupts microbial balance and weakens the gut barrier, paving the way for pathology.
To forge a complete connection, human intervention trials were essential. A landmark six-month randomized controlled feeding study examined dietary fat’s influence on gut microbiota. Results confirmed that elevated fat intake correlated with detrimental shifts in the gut microbiome and heightened proinflammatory markers circulating in the blood. Notably, this trial did not focus exclusively on saturated fats from animal sources; instead, it substituted refined carbohydrates—like white rice and wheat flour—with refined plant oils such as soybean oil.
These insights carry broad implications. Nations undergoing dietary Westernization should be counseled to avoid ramping up fat consumption. Those already entrenched in high-fat dietary norms might benefit from strategies to reduce overall fat intake, thereby supporting gut microbiome health and barrier integrity.
Key Insights on Protecting Your Gut Barrier
In summary, ubiquitous drugs including aspirin, ibuprofen, and alcohol can elevate intestinal permeability, facilitating the entry of harmful agents into the bloodstream. This process may ignite systemic inflammation or provoke allergic responses.
A weakened intestinal barrier associates with serious ailments like inflammatory bowel disease, food allergies, and cardiometabolic diseases, positioning it as a prime focus for preventive measures and treatments.
Western diets high in fats detrimentally alter the gut microbiome and impair barrier function. Conversely, lowering fat consumption and steering clear of damaging agents can preserve or rehabilitate intestinal health effectively.
Maintaining a robust gut barrier is foundational to long-term wellness. By making informed choices about medications, alcohol, and especially dietary fats, individuals can mitigate risks and foster a healthier digestive ecosystem. This approach not only addresses leaky gut but also supports broader metabolic and immune functions.









