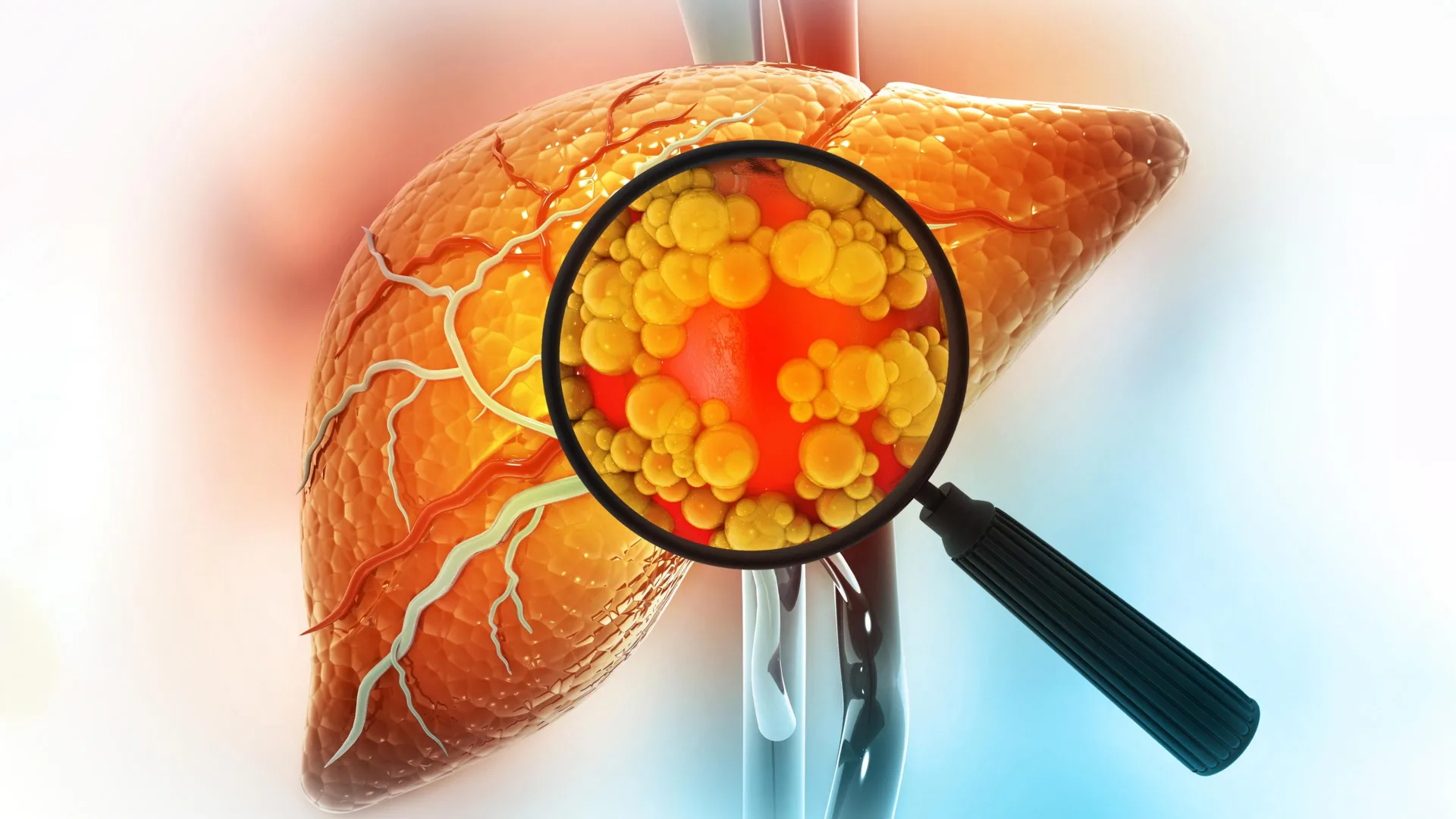
Consuming a diet rich in fats stands out as one of the most significant factors elevating the risk of liver cancer. Recent findings from researchers at MIT provide crucial insights into the mechanisms behind this phenomenon, demonstrating how diets loaded with fats can profoundly modify liver cells, thereby heightening the chances of cancer development.
The scientific team observed that prolonged exposure of the liver to a high-fat diet prompts mature liver cells, known as hepatocytes, to undergo a substantial transformation. Rather than maintaining their fully differentiated state, these cells revert to a more primitive condition resembling stem cells. This adaptive shift enables them to endure the pressures imposed by excessive fat buildup, but it simultaneously renders them more prone to malignant transformation over extended periods.
‘When cells face repeated exposure to a stressor like a high-fat diet, they activate survival mechanisms that enhance their resilience, yet this comes at the cost of greater vulnerability to tumor initiation,’ explains Alex K. Shalek, who serves as director of the Institute for Medical Engineering and Sciences (IMES), holds the J. W. Kieckhefer Professorship in IMES and the Department of Chemistry, and is affiliated with the Koch Institute for Integrative Cancer Research at MIT, the Ragon Institute of MGH, MIT, and Harvard, as well as the Broad Institute of MIT and Harvard.
Furthermore, the investigators pinpointed key transcription factors that orchestrate this cellular reprogramming. These molecular players hold promise as future therapeutic targets for medications aimed at mitigating tumor risk in susceptible individuals.
The study’s senior authors include Shalek; Ömer Yilmaz, an associate professor of biology at MIT and member of the Koch Institute; and Wolfram Goessling, co-director of the Harvard-MIT Program in Health Sciences and Technology. The research appeared in the journal Cell on December 22. Constantine Tzouanas, a graduate student at MIT; Jessica Shay, formerly a postdoc at MIT; and Marc Sherman, a postdoc at Massachusetts General Brigham, share lead authorship on the paper.
How Diets High in Fat Induce Liver Cell Dedifferentiation
Diets abundant in fats often trigger inflammatory responses and lipid buildup within the liver, culminating in steatotic liver disease. This pathological state can also stem from chronic metabolic burdens, such as excessive alcohol intake, and may advance to cirrhosis, liver dysfunction, and eventually hepatocellular carcinoma.
In their investigation, the researchers sought to elucidate the molecular responses of liver cells to high-fat diet exposure, particularly tracking alterations in gene expression as the pathological process evolves.
To delve into this, the group administered a high-fat diet to mice and employed single-cell RNA-sequencing techniques to profile liver cells during critical phases of disease progression. This methodology enabled precise monitoring of gene activity fluctuations from initial inflammation through fibrosis and onward to malignancy.
In the initial stages, hepatocytes upregulated genes that bolster survival under duress. These encompassed protective mechanisms against apoptosis and stimulators of proliferation. Concurrently, genes critical for core liver operations—such as metabolic processing and protein export—were progressively suppressed.
‘This pattern suggests a strategic compromise, where individual cells prioritize personal survival in a hostile milieu over the organ’s collective physiological duties,’ notes Tzouanas.
Certain genetic adaptations manifested rapidly, whereas others progressed gradually. For instance, the downregulation of metabolic enzymes occurred over an extended timeframe. By the experiment’s conclusion, virtually every mouse on the high-fat regimen had succumbed to liver tumors.
Why Dedifferentiated Liver Cells Accelerate Tumorigenesis
The findings revealed that hepatocytes in a less differentiated state are particularly susceptible to oncogenic mutations, facilitating rapid cancer progression.
‘These cells have preemptively activated the genetic programs necessary for malignancy. They’ve diverged from their mature phenotype, which typically constrains proliferative capacity,’ Tzouanas elaborates. ‘Consequently, upon acquiring a deleterious mutation, the cell is primed for unchecked expansion, embodying key cancer characteristics from the outset.’
The study illuminated several genes that drive this reversion to an immature phenotype. Notably, a drug targeting the thyroid hormone receptor—one of these genes—has gained approval for managing advanced steatotic liver disease, specifically MASH fibrosis. Additionally, an activator of another identified enzyme, HMGCS2, is undergoing clinical evaluation for steatotic liver conditions.
A particularly intriguing candidate is the transcription factor SOX4, which is predominantly expressed during embryonic development and in select adult tissues excluding the liver. Its emergence in stressed hepatocytes underscores a significant deviation from normal cellular identity.
Validation in Human Liver Pathologies
Building on murine models, the team validated these observations in human specimens by analyzing liver biopsies from patients across various disease stages, including pre-cancerous phases.
The human data paralleled the mouse results strikingly: genes underpinning mature liver functions waned, while those associated with primitive states surged. Moreover, these expression profiles proved prognostic, correlating with survival post-tumor diagnosis.
‘Individuals exhibiting elevated levels of these survival-promoting genes, activated by high-fat exposure, experienced shorter survival after tumor onset,’ Tzouanas observes. ‘Similarly, diminished expression of genes vital to hepatic functions predicted poorer outcomes.’
Whereas tumors arose in mice within roughly one year, the human trajectory is projected to span approximately two decades, modulated by dietary habits, alcohol consumption, viral hepatitis, and other accelerators that similarly destabilize hepatocyte maturity.
Reversibility of Diet-Induced Liver Alterations
Moving forward, the researchers intend to assess if high-fat diet-induced cellular reprogramming is reversible. Upcoming experiments will evaluate the impacts of dietary normalization or interventions like GLP-1 receptor agonists on restoring hepatocyte functionality.
They will also probe the therapeutic potential of the discovered transcription factors to halt progression from fibrosis to cancer.
‘With these novel molecular insights and a deeper grasp of the underlying pathophysiology, we can pursue innovative strategies to enhance patient prognoses,’ Shalek concludes.
Funding for this work was supported by sources including the Fannie and John Hertz Foundation Fellowship, National Science Foundation Graduate Research Fellowship, National Institutes of Health grants, and the MIT Stem Cell Initiative via Foundation MIT.