What’s Really Happening Inside Your Body
You begin your day feeling perfectly normal. Your abdomen is flat, your pants fasten without any struggle, and optimism fills your thoughts. However, as noon approaches, everything changes dramatically. Before you know it, you find yourself discreetly loosening your waistband while seated at your workstation. Your midsection suddenly resembles that of someone well into pregnancy. Even worse, you experience real discomfort, potentially accompanied by actual pain.
Does this sequence sound all too familiar? This recurring cycle represents one of the most frequent issues reported by women grappling with various gastrointestinal challenges. Importantly, this phenomenon is far from arbitrary. There exist concrete, addressable factors driving why your abdominal distension follows such a consistent daily trajectory.
Bloating that builds progressively as the day advances typically indicates how your gastrointestinal tract manages the buildup of ingested material and the subsequent microbial breakdown processes. Upon waking, your digestive apparatus has benefited from an extended period—typically 8 to 12 hours—of rest, allowing it to fully handle the previous day’s intake. Consequently, your stomach remains largely vacant, with gas generation kept to a minimum, fostering a sense of tranquility. Keep in mind, though, that if you awaken already distressed, this suggests a separate underlying issue requiring distinct attention.
Nevertheless, once you commence consuming food during the day, a series of physiological events unfolds:
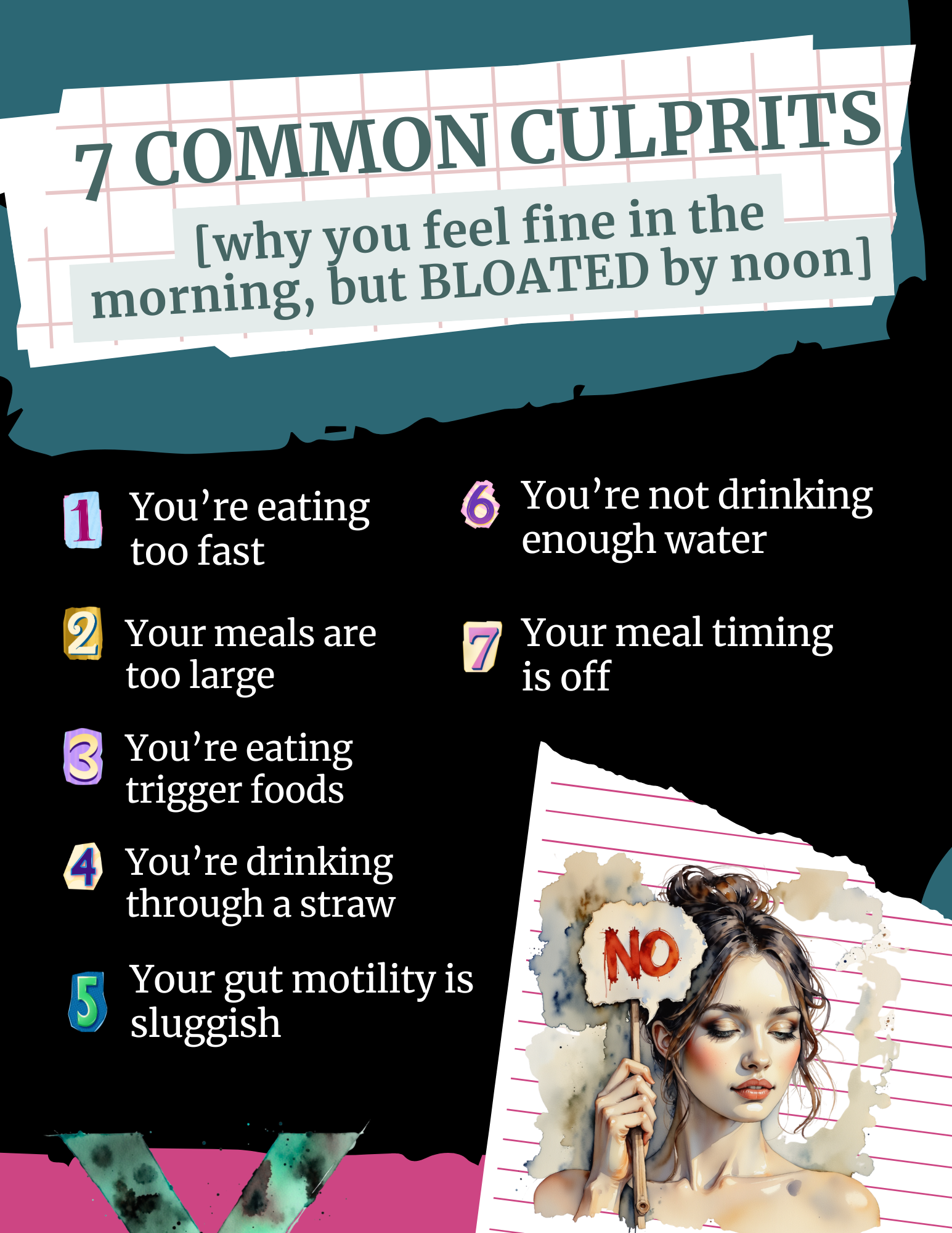
The Primary Contributors to Daily Bloating
As meals are introduced, residue begins to gather within your gastrointestinal pathway. Every portion consumed must undergo disassembly, assimilation, and propulsion through the system. Should any segment of this mechanism operate suboptimally, ingested matter starts to congest, leading to delays.
Simultaneously, microbial activity in the intestines ramps up. As nutrients traverse the lower gut, resident bacteria metabolize specific elements, especially complex sugars and fibrous materials. This metabolic process yields gases as inevitable byproducts. Greater food volumes translate to heightened fermentation activity, resulting in elevated gas levels.
Additionally, the output of digestive enzymes may wane as the day progresses. This decline is particularly pronounced among individuals under pressure or consuming meals hastily. Reduced enzyme availability hampers effective nutrient breakdown. Studies featured in the American Journal of Gastroenterology reveal that individuals suffering from functional abdominal distension exhibit markedly higher intestinal gas formation and compromised gas evacuation relative to those without symptoms.

1. Consuming Meals at Excessive Speeds
Rapid eating leads to inadvertent air ingestion alongside insufficient mastication. Consequently, bigger chunks of food arrive in the stomach and beyond, demanding extra effort from the digestive organs to pulverize them. This extra labor generates additional gases and impedes overall transit efficiency. Personally, I once devoured lunches at my desk amid work demands, only to puzzle over the explosive sensations by mid-afternoon.
2. Overly Substantial Meal Portions
Massive servings strain the digestive capacity. The body possesses finite enzyme production limits per session. Overloading with excessive quantities leaves remnants inadequately processed, lingering in the intestines. These leftovers serve as prime substrates for bacterial proliferation, fueling fermentation and gas buildup.
3. Incorporation of Problematic Food Items
Specific edibles are well-known for provoking substantial gas formation:
- High-FODMAP items such as onions, garlic, legumes, and select fruits
- Vegetables from the cruciferous family, including broccoli, cauliflower, and Brussels sprouts
- Dairy if lactose digestion is impaired
- Synthetic sugar substitutes like sorbitol and xylitol
- Fizzy drinks
- Items rich in resistant starch
4. Using Straws for Beverages
Sipping through straws prompts additional air swallowing, exacerbating distension. Similar effects arise from gum chewing or conversing during meals.
5. Impaired Intestinal Propulsion
Delayed movement of contents through the gut prolongs exposure to fermentative bacteria, amplifying gas and swelling. Factors influencing propulsion speed encompass:
- Chronic stress
- Sedentary habits
- Inadequate fluid intake
- Pharmacological influences
- Conditions such as small intestinal bacterial overgrowth or irritable bowel syndrome
6. Insufficient Hydration Levels
Counterintuitively, dehydration promotes fluid retention and puffiness. Proper water intake is vital for facilitating material transport and enabling enzyme efficacy throughout the tract.
7. Inappropriate Meal Scheduling
Scheduling intakes too closely denies the system recovery intervals between loads. Late-evening consumption further burdens the gut during its intended downtime.
The Impact of Stress on Digestion
Psychological tension profoundly disrupts gastrointestinal operations. Under duress, circulation shifts from digestive tissues to skeletal muscles, embodying the classic fight-or-flight mechanism. This redirection signals the body to favor survival actions over nutrient processing.
Key repercussions include:
- Diminished circulation for enzyme synthesis
- Reduced propulsion velocity
- Disrupted microbial equilibrium
- Elevated gut lining permeability
Mornings often feel manageable since cumulative stressors remain low. By afternoon, however, occupational demands, time constraints, and divided attentions trigger these responses. Scientific inquiries confirm that tension reshapes microbial communities and heightens abdominal sensitivity, both fueling distension.
Practical Strategies to Counteract This Pattern
Fortunately, grasping these dynamics empowers you to break the cycle effectively. Below are proven tactics to implement:
1. Initiate the Day with Digestive Priorities
Avoid omitting the first meal or rushing it en route. Allocate time for a seated, nutritionally balanced intake featuring proteins and beneficial lipids. This foundational step primes your system for sustained performance.
2. Opt for Modest, Regular Portions
Shift from infrequent large helpings to smaller, spaced-out servings. This approach delivers digestible quantities without overload. Crucially, maintain 90-120 minute gaps to permit the migrating motor complex—essential for cleansing the gut—to function unimpeded.
3. Prioritize Thorough Mastication
Target 20-30 chews per mouthful. Oral breakdown initiates digestion, easing subsequent stages and minimizing downstream burdens.
4. Practice Attentive Eating
Eliminate distractions like devices or screens. Concentrate solely on the meal. Tension or inattention during intake compromises processing efficiency.
5. Pinpoint Personal Food Sensitivities
Maintain a detailed log of consumables and resulting sensations. Identify recurrent culprits, as tolerances vary widely among individuals.
6. Incorporate Movement
Gentle activity post-meals enhances transit. A brief stroll yields noticeable improvements.
7. Ensure Consistent Hydration
Target water volumes equaling half your body weight in ounces daily. Distribute intake evenly, sipping separately from meals to avoid dilution effects.
8. Address Stress Proactively
Though challenging, tension mitigation proves essential. Explore techniques like diaphragmatic breathing, mindfulness practices, yoga, or scheduled pauses that resonate with you.
9. Explore Supportive Supplements
Options such as enzyme formulations, hydrochloric acid boosters, or herbal bitters may aid function. Consult experts to tailor selections to your needs.

The Crucial Role of Food Quality
An underemphasized aspect involves ingredient purity. Ultra-processed items, chemical additives, and subpar fats incite inflammatory responses and processing difficulties. Unfamiliar components challenge recognition and handling.
Conversely, unadulterated, integral foods supply the precise nutrients required for seamless operations. Adopting this shift often delivers the swiftest relief from symptoms.
Indicators for Professional Evaluation
Persistent escalation may signal deeper pathologies demanding investigation:
- Small intestinal bacterial overgrowth, where surplus microbes prematurely degrade carbs, peaking distension post-carbohydrate meals. Morning comfort contrasting afternoon agony strongly suggests this.
- Intolerances to gluten, histamines, or other elements beyond dairy.
- Motility impairments prolonging retention times.
- Microbial dysbiosis elevating gas yields.
If foundational adjustments fail to resolve issues, seek guidance from gut-savvy practitioners.
A Comprehensive Reset Methodology
Occasionally, a full system reboot proves most efficacious. Structured programs emphasize respite from irritants alongside sustenance from restorative edibles. Sample protocols feature:
- Macronutrient equilibrium for glycemic steadiness
- Anti-inflammatory agents like turmeric and ginger
- Proteins promoting fullness and mucosal integrity
- Salubrious lipids supporting endocrinology
- Measured servings preventing overload
Participants frequently report diminished swelling within days of adherence. This pattern communicates that your physiology signals suboptimal states. Reassuringly, innate healing capacities await appropriate facilitation.
Sustaining Long-Term Improvements
Refuse to normalize daily distension. Commence with fundamentals:
- Pace intake deliberately
- Masticate meticulously
- Hydrate diligently
- Regulate tension
- Monitor trends astutely
Subsequently, evaluate structured interventions incorporating extensive recipes, tracking frameworks for trigger detection, and expert support. Midday discomfort mimicking advanced gestation need not define your routine. Heed your body’s cues and respond decisively.