Exploring Mushrooms and Their Potential Role in Prostate Cancer Management
Various types of mushrooms, including reishi varieties, extracts derived from shiitake mushrooms, and even powdered forms of common white mushrooms, have sparked interest regarding their possible benefits for individuals battling cancer. Regular consumption of mushrooms has been suggested to enhance overall health, boost physical fitness, elevate mood, and potentially extend lifespan, but substantial scientific backing for these claims remains somewhat limited, particularly in rigorous human trials conducted under modern research standards.
One specific substance known as lentinan, which is isolated from shiitake mushrooms, has garnered attention in medical research. Producing just one ounce of this compound requires processing an astonishing quantity—approximately 400 pounds of fresh shiitake mushrooms, equivalent to roughly 2,000 cups. In experimental settings, scientists administered this extract directly into the bloodstream of cancer patients to evaluate its effects. A meta-analysis combining data from twelve modest-sized clinical trials revealed that incorporating lentinan alongside standard chemotherapy protocols for lung cancer patients led to a notable enhancement in the objective response rates. This metric typically refers to measurable outcomes like tumor size reduction. However, the ultimate goals for patients extend beyond mere tumor shrinkage to encompass extended survival periods and improved daily living standards. Does this compound truly extend life or elevate quality of life for those affected?
Patients receiving lentinan experienced fewer adverse effects from chemotherapy, particularly reduced damage to the gastrointestinal tract and bone marrow, which could independently justify its inclusion in treatment plans. Yet, the critical question persists: does it meaningfully prolong life? Initial excitement arose from findings suggesting lentinan could substantially boost survival rates in certain leukemias. Further investigation confirmed that combining it with conventional therapies extended average survival times, diminished cancer-related muscle wasting known as cachexia, and enhanced observable health markers. Upon closer examination, however, these promising outcomes were observed in brown Norwegian rats, limiting their direct applicability to human medicine unless one is treating rodents or working in veterinary oncology.
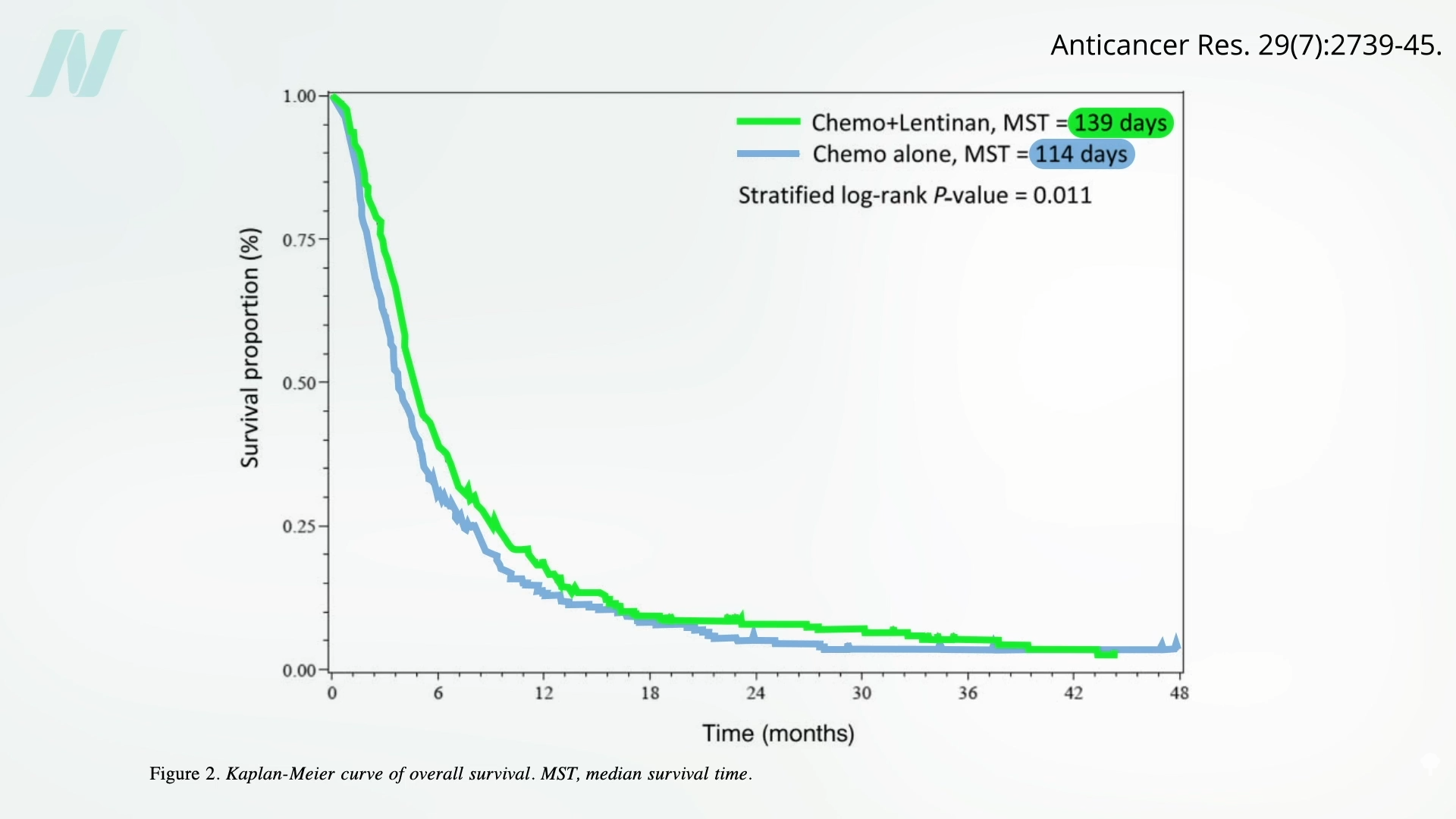
A broader review encompassing 17 genuine human clinical trials indicated modest improvements in one-year survival rates among patients with advanced cancers, though no substantial differences emerged by the two-year mark. Even aggregated analyses claiming significant survival advantages with lentinan often hinge on statistical significance rather than clinically transformative differences. Visual inspection of survival curve graphs reveals curves that are nearly indistinguishable, with lentinan extending average survival by a mere 25 days—a figure that, while positive, warrants cautious interpretation and skepticism toward overly optimistic commercial promotions of medicinal mushrooms.
Since lentinan requires intravenous administration, attention has turned to oral mushroom extract supplements available over the counter. Shiitake extracts, marketed online for prostate cancer management at costs around $300 monthly, raise questions about their true efficacy. Observational data suggests that men who frequently include mushrooms in their diets face a reduced risk of developing prostate cancer, an association persisting even after accounting for variables like lower meat intake or higher fruit and vegetable consumption. This prompts consideration of shiitake extracts as a potential intervention. Regrettably, clinical testing reveals them to be ineffective as standalone treatments for established prostate cancer in humans. Researchers emphasized how straightforward it is to rigorously test such complementary and alternative medicine claims, advocating for evidence-based validation before consumers invest heavily in unverified or refuted remedies.
Reishi mushrooms, revered in some traditions as the ‘mushroom of God’ or ‘mushroom of immortality,’ have also undergone scrutiny. Clinical evaluations concluded with no observable anticancer effects, lacking even partial tumor responses in participants. Perhaps the focus on exotic varieties overlooks simpler options. Extracts from ordinary white button mushrooms demonstrate the ability to eliminate prostate cancer cells in laboratory cell cultures, similar to more exotic types. However, petri dish success does not guarantee real-world human efficacy, necessitating direct patient studies.
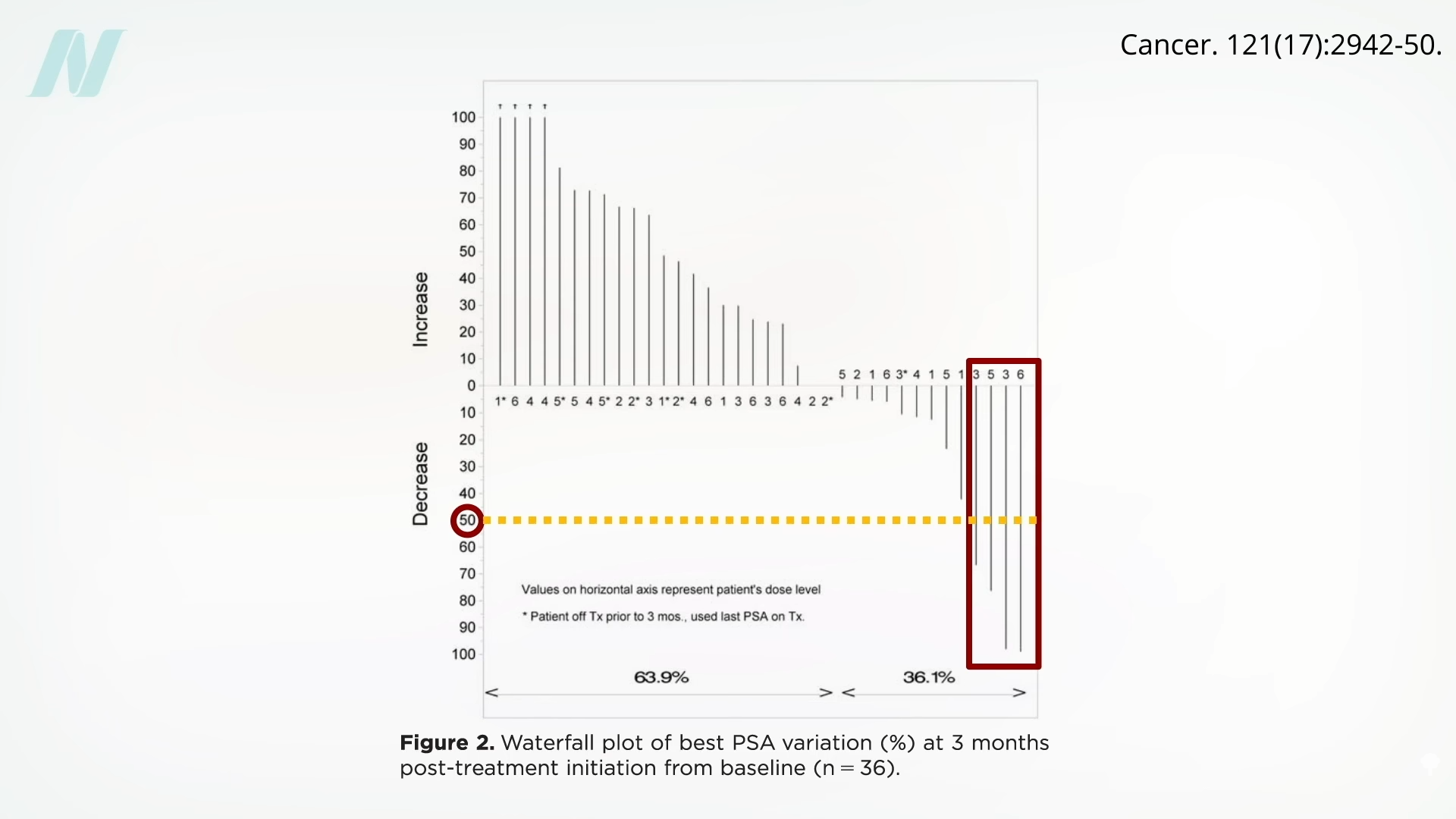
A particularly compelling investigation utilized straightforward, whole white button mushrooms—dried and powdered—without relying on proprietary formulations. Participants consumed amounts equivalent to half a cup up to one and a half cups of fresh mushrooms daily, a practical and achievable quantity for regular dietary incorporation. The study targeted men diagnosed with biochemically recurrent prostate cancer, a condition where malignancy reemerges post-prostatectomy or radiation therapy, as indicated by escalating prostate-specific antigen (PSA) levels signaling disease progression.
Among the 26 men who received the mushroom powder supplementation, four demonstrated clear positive responses, characterized by PSA reductions exceeding 50% following the intervention’s commencement. This outcome highlights the potential responsiveness in a subset of patients.
Examining pre-treatment trends for these responders reveals compelling patterns. For instance, Patient 2 exhibited a sharp, exponential rise in PSA over the preceding year, which dramatically reversed upon initiating mushroom intake, plummeting to undetectable levels and remaining suppressed thereafter. Patient 1 mirrored this trajectory with a sustained decline. Patient 4 achieved a temporary partial reduction before progression resumed, while Patient 3 showed a delayed but notable partial response.
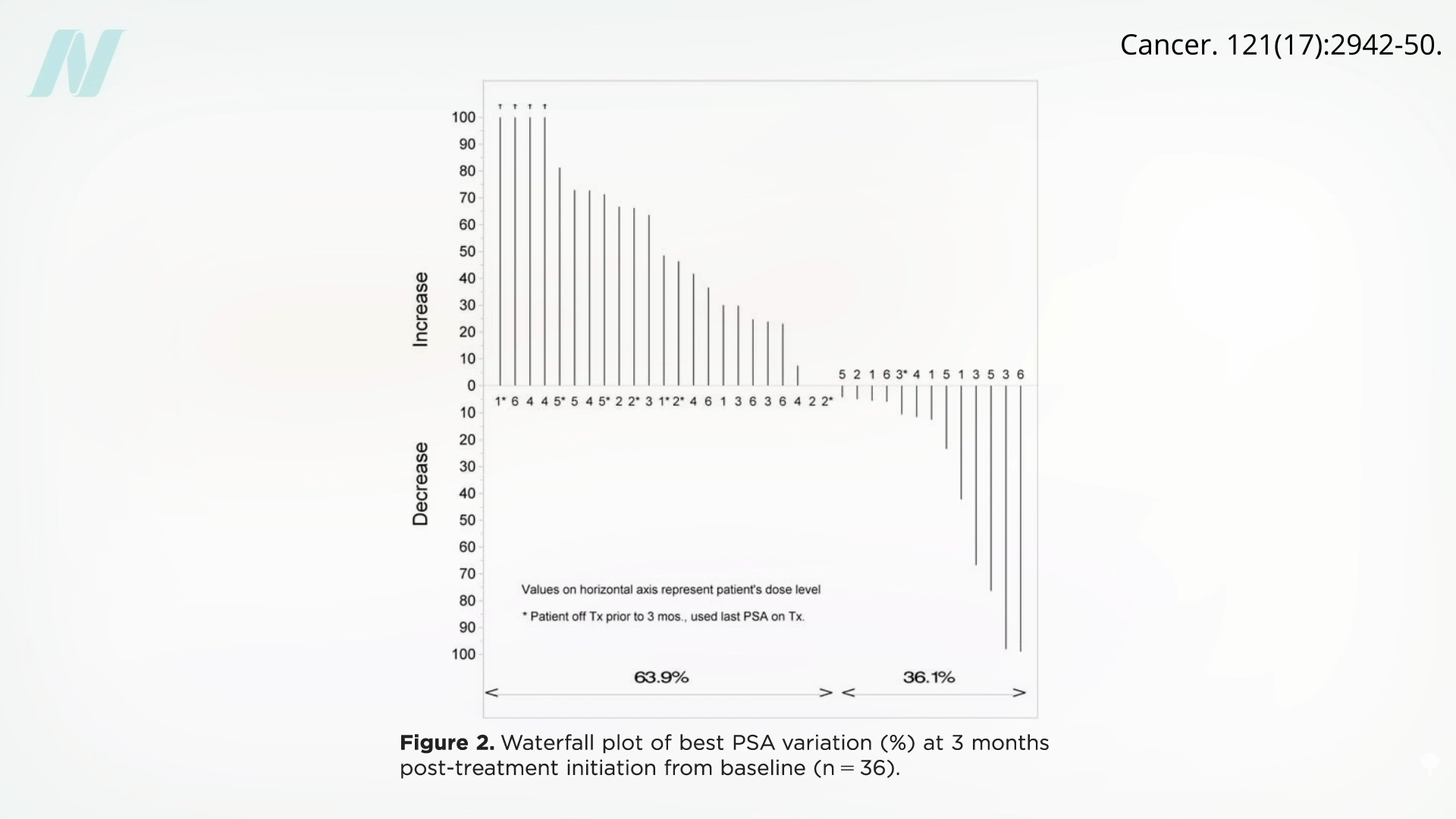
In the majority of participants, PSA levels continued their upward trajectory without interruption. Nonetheless, even a modest probability—such as 1 in 18—of achieving a sustained, complete response, as observed in standout cases like Patients 1 and 2, presents an intriguing prospect. These individuals enjoyed prolonged periods of undetectable PSA, intimating possible complete cancer remission.
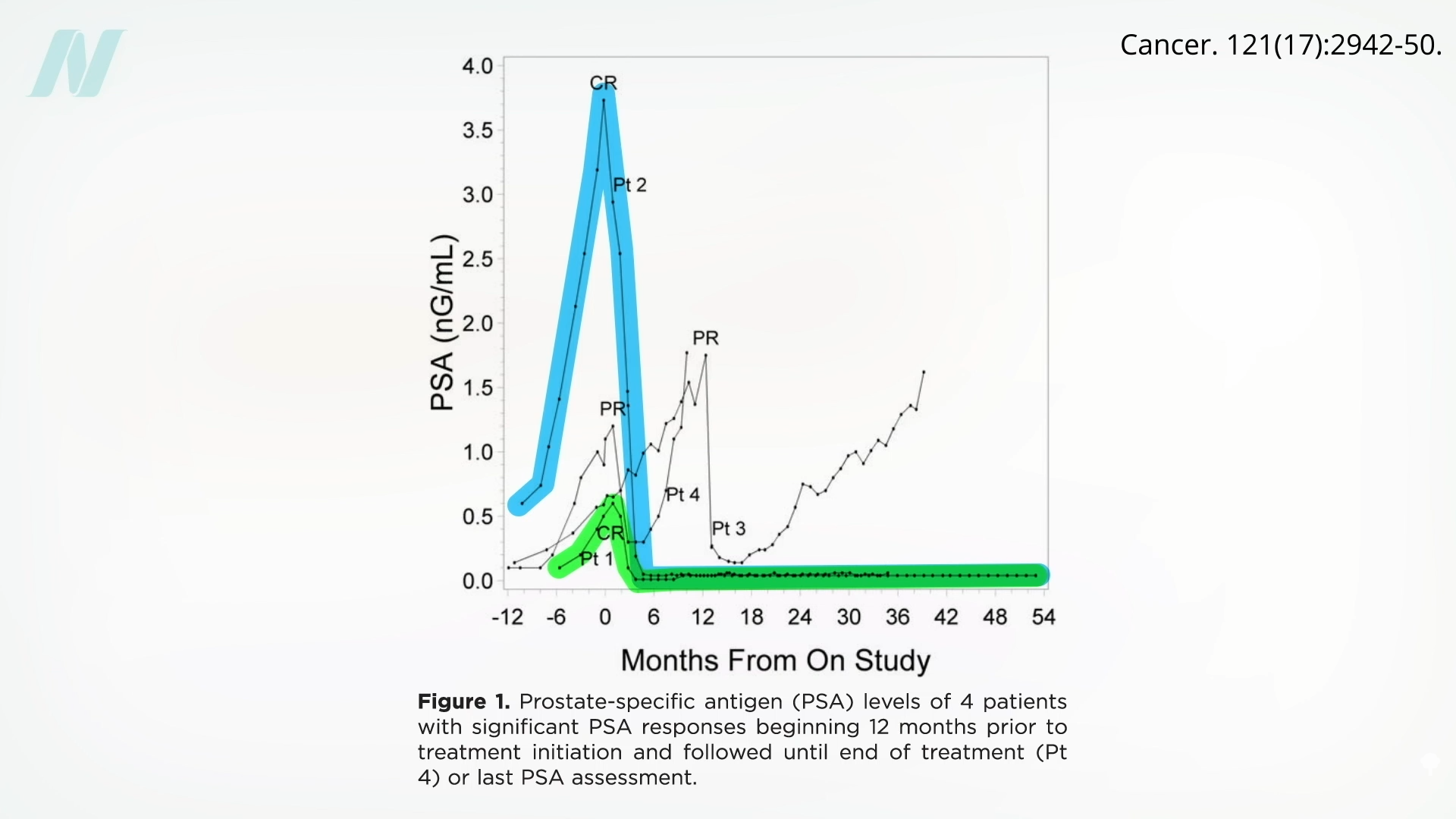
This approach contrasts sharply with high-risk chemotherapies, offering instead a low-stakes addition of affordable, palatable white button mushrooms to one’s daily routine. Although the absence of a control group introduces uncertainty—potentially attributing outcomes to chance—persistently rising PSA in post-surgical patients reliably forecasts progression. The risk of trialing mushrooms appears negligible, with no apparent downsides to their dietary inclusion.
For the two patients achieving undetectable PSA, the implications are profound: despite prior surgical excision of the primary tumor and prostate gland, followed by radiation to eradicate residuals, cancer markers surged—only to abate completely upon mushroom introduction. This underscores the value of accessible, whole-food interventions in oncology supportive care.
Key Insights on Mushrooms in Cancer Contexts
- Despite enthusiastic marketing, robust human clinical evidence supporting expansive health benefits of medicinal mushrooms remains scarce.
- Shiitake-derived lentinan offers minor advantages, including marginal survival extensions and lessened chemotherapy side effects, predominantly evidenced in animal models or limited-scale human trials.
- Supplements from shiitake or reishi fail to demonstrate reliable anticancer activity in human prostate cancer trials, notwithstanding in vitro or preclinical promise.
- Everyday white button mushrooms, consumed in feasible dietary doses, exhibited capacity to substantially lower PSA in a preliminary prostate cancer cohort, meriting expanded controlled investigations.
Incorporating mushrooms into a balanced diet represents a simple, evidence-informed strategy potentially aiding prostate health. While not a standalone cure, their profile of safety and accessibility encourages broader exploration in nutritional oncology research. Ongoing studies may further elucidate mechanisms, such as bioactive compounds influencing hormone pathways or immune modulation, that underpin observed PSA dynamics. Men navigating prostate cancer diagnoses or recurrence might consider discussing practical mushroom integration with healthcare providers, alongside conventional therapies, to optimize outcomes holistically.









