Approximately fifty million individuals in the United States are affected by arthritis, with osteoarthritis specifically targeting the knee being the predominant variety and a primary contributor to disability among the population. The underlying mechanisms of this condition involve multiple inflammatory processes that drive both its initiation and worsening over time. Consequently, a range of anti-inflammatory dietary options have undergone rigorous scientific evaluation to determine their potential efficacy. For instance, the consumption of strawberries has demonstrated the ability to lower levels of tumor necrosis factor, a key inflammatory agent circulating in the bloodstream. Nevertheless, reductions in such markers do not always correspond to tangible clinical benefits for patients.
Exploring Berries and Other Foods for Inflammation Control
Consider the case of cherry juice, which has been observed to diminish concentrations of C-reactive protein, another prominent indicator of inflammation within the body. Despite this biochemical effect, it did not succeed in alleviating pain or other associated symptoms in individuals suffering from knee osteoarthritis. Researchers involved in the study suggested that it offered some degree of symptom relief; however, this improvement was only evident when comparing pre- and post-intervention measurements after six weeks of consumption. Crucially, it performed no superior to a placebo treatment, implying that the benefits were indistinguishable from simply doing nothing at all. While cherries may provide assistance in managing gout, a distinct form of arthritis, they fell short in addressing osteoarthritis effectively.
In contrast, strawberries exhibited more promising outcomes by not only reducing inflammation but also delivering a measurable analgesic impact. A carefully designed randomized, double-blind, crossover clinical trial confirmed that incorporating dietary strawberries led to a statistically significant reduction in reported pain levels among participants. Pharmaceutical interventions targeting tumor necrosis factor are currently accessible on the market, though they come at an exorbitant annual expense of roughly $40,000. Given such a steep price tag, one would anticipate substantial efficacy, yet these medications are accompanied by severe adverse effects, including a heightened risk of particularly aggressive lymphomas. Opting for strawberries appears to be a far more prudent and cost-effective strategy in comparison.
The rationale for investigating berries stems from laboratory evidence showing their potent anti-inflammatory properties. When participants consumed the equivalent of about one cup of blueberries or two cups of strawberries each day, subsequent analysis of their blood applied to cell cultures in petri dishes revealed markedly reduced inflammatory responses compared to blood from those given placebo berries.
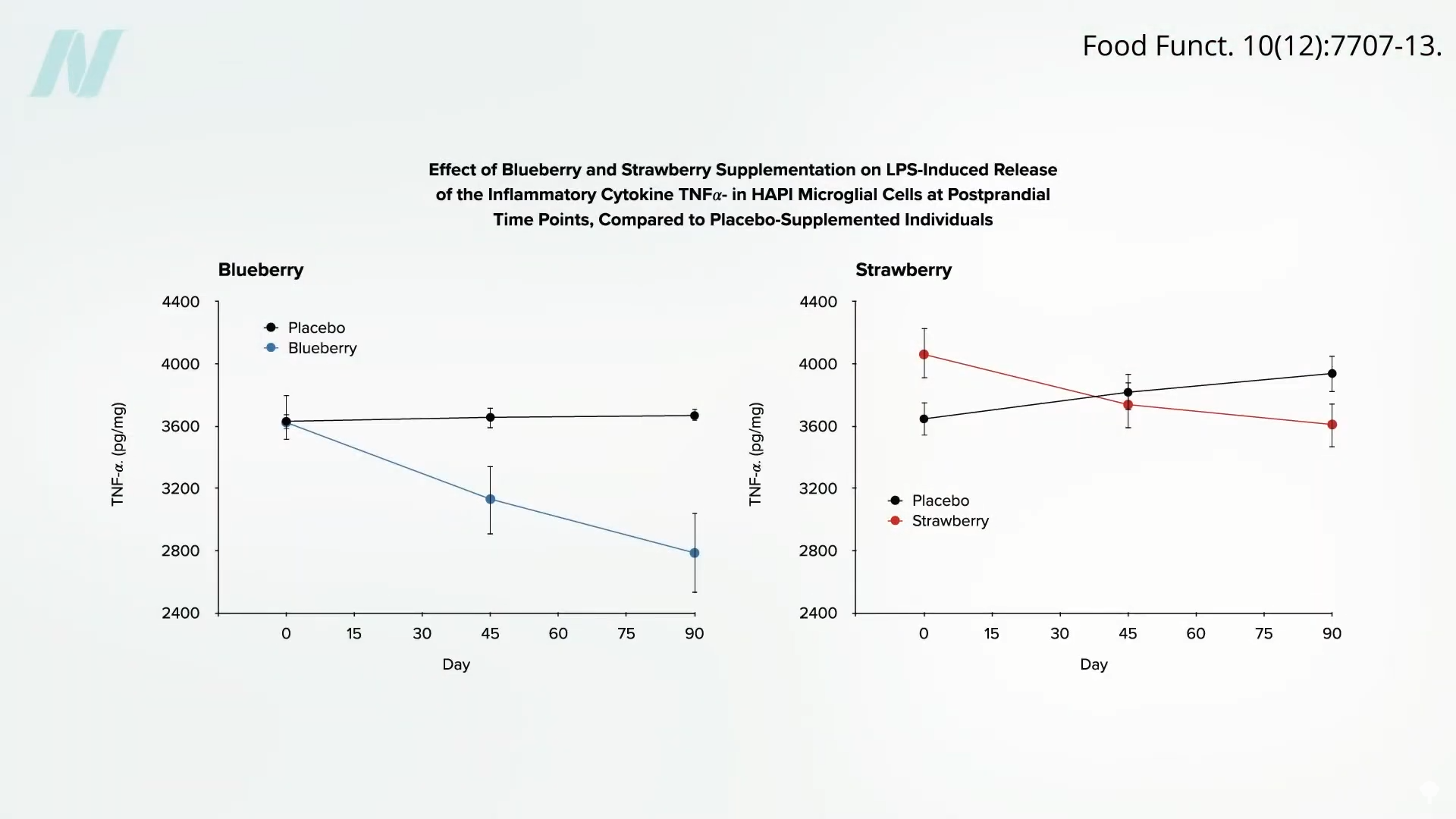
Notably, this suppressive effect on inflammation intensified progressively with continued daily intake, indicating that sustained berry consumption could yield accumulating benefits over time. This prompts the question: have other dietary components been subjected to similar rigorous testing methodologies?
Investigating Extracts from Grapes and Olives
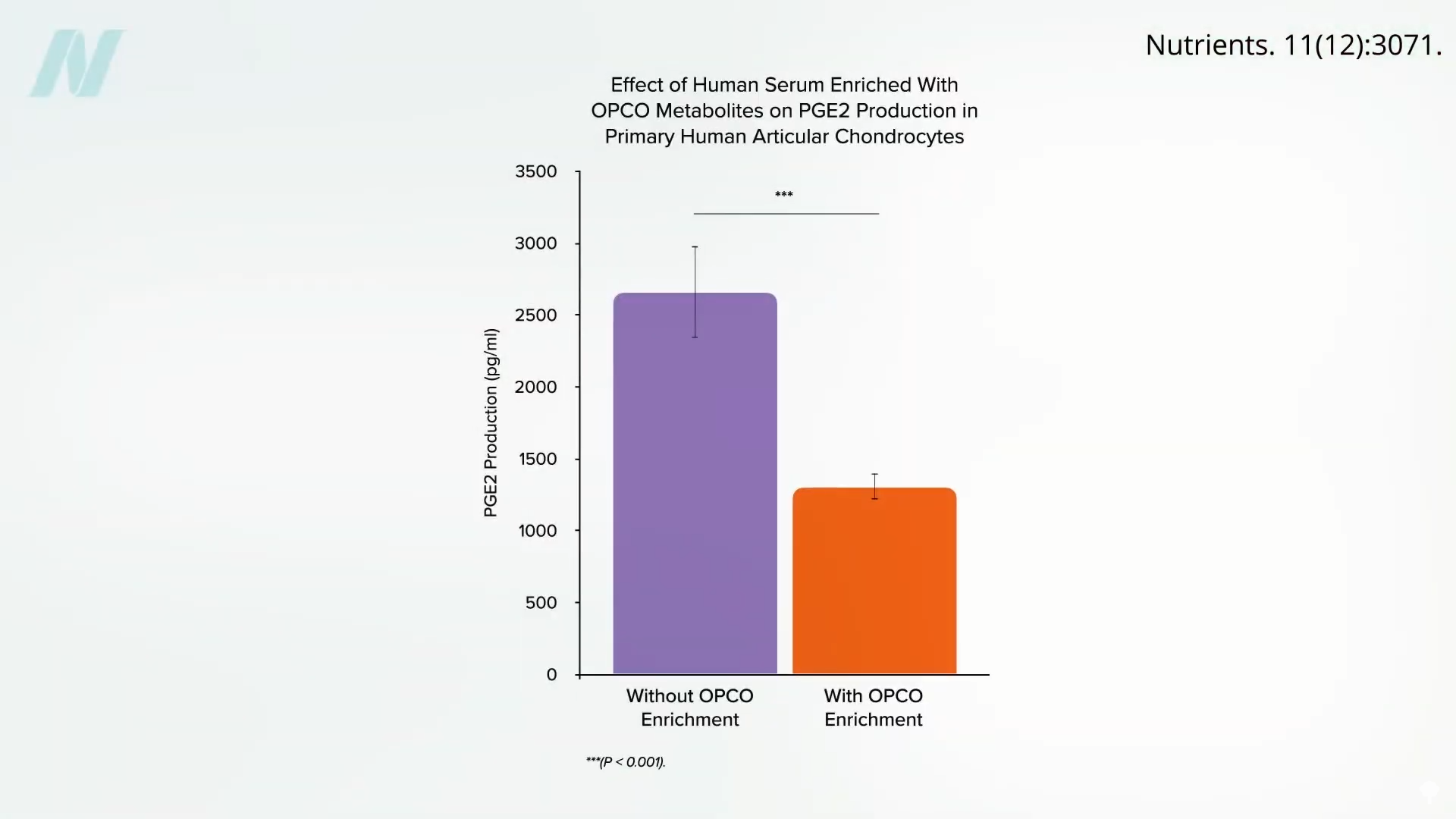
Scientists in France obtained cartilage samples from patients undergoing knee replacement procedures and subsequently exposed these tissues to blood drawn from volunteers who had ingested a substantial quantity of a combined grapeseed and olive extract. The results indicated a pronounced decline in inflammatory activity within the cartilage samples.
Although no clinical trials have yet evaluated grapeseed extracts directly in human arthritis patients, an olive-derived extract has been demonstrated to effectively lessen pain and enhance performance of daily activities in those with osteoarthritis. This raises the possibility that incorporating olive oil into one’s regular diet might confer similar advantages. However, the extract in question was derived from freeze-dried olive vegetation water, which constitutes the aqueous remnants after oil extraction from olives, encompassing all water-soluble bioactive compounds absent in the pure oil itself.
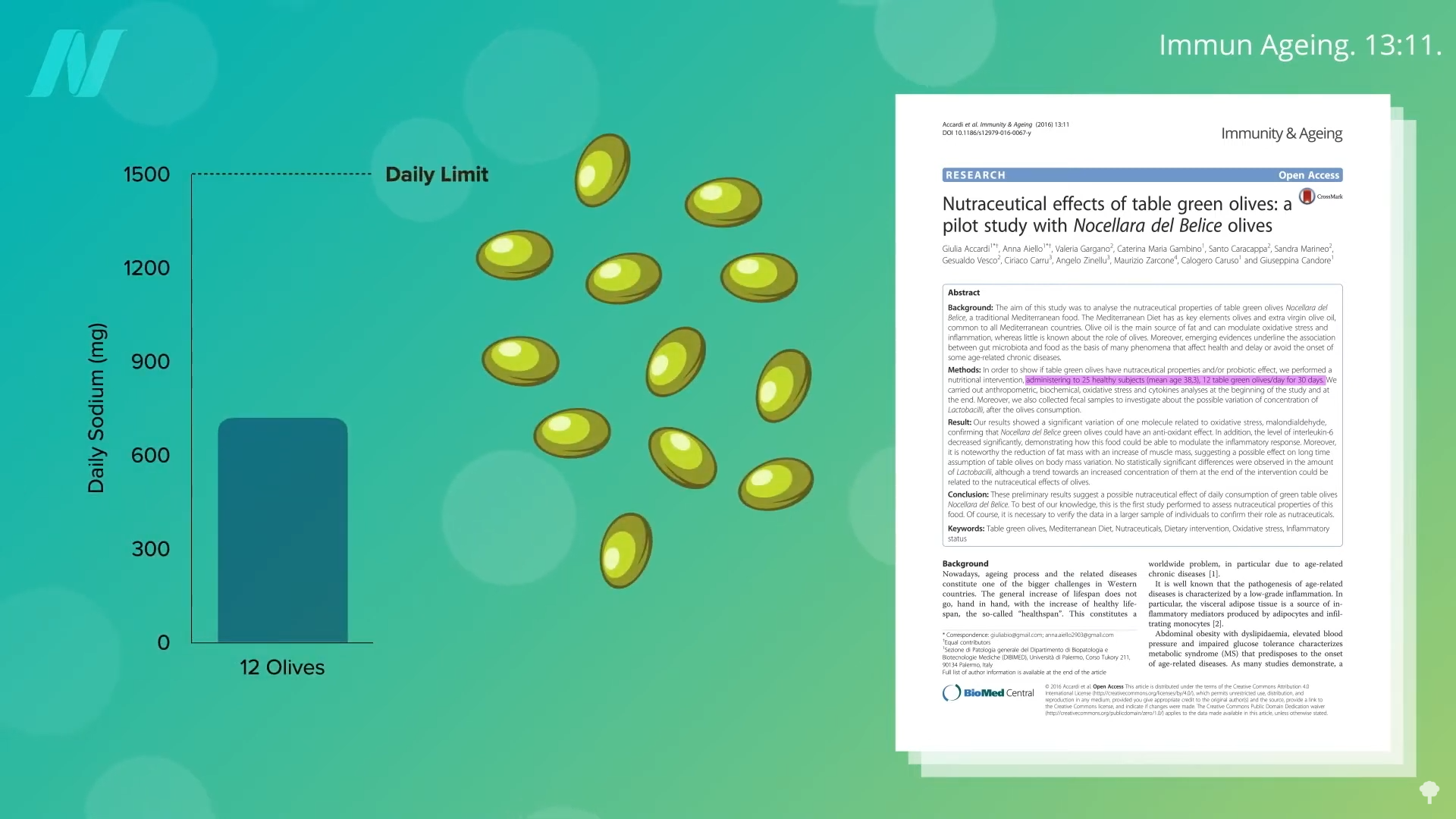
Administering whole olives—specifically a dozen large green ones daily—has been linked to reductions in certain inflammatory mediators. Yet, a comprehensive systematic review and meta-analysis of existing literature concludes that olive oil, when consumed independently, fails to deliver discernible anti-inflammatory advantages in humans. Studies attributing extraordinary anti-inflammatory prowess to extra virgin olive oil often rely on animal models, particularly rodents. In human subjects, extra virgin olive oil shows no superiority over butter in modulating inflammation and may even underperform compared to coconut oil in some assessments.
Does this suggest that whole olives should be the preferred choice? Regrettably, consuming a dozen olives can account for nearly half of the recommended daily sodium allowance, posing a concern for sodium intake management.
Extra virgin olive oil has also been tested for fibromyalgia, a condition involving widespread pain and tenderness, but it did not demonstrate meaningful improvements in symptoms. On a more positive note, it outperformed canola oil in mitigating manifestations of inflammatory bowel disease. Despite extensive searches, no investigations were identified that specifically examined the oral consumption of olive oil in the context of arthritis treatment. So, what accounts for the focus on olive oil’s potential rivalry with arthritis medications? The answer lies in its application as a topical agent.
Topical Application: Olive Oil Outperforms Ibuprofen Gel
In a double-blind, randomized clinical trial, topical virgin olive oil was directly compared to a pharmaceutical gel formulated with an ibuprofen-like nonsteroidal anti-inflammatory drug for the management of knee osteoarthritis. Participants applied just one gram of olive oil—equivalent to less than a quarter of a teaspoon—three times per day, at a nominal daily cost of under three cents. Remarkably, the olive oil proved significantly more effective than the drug gel in diminishing pain intensity.
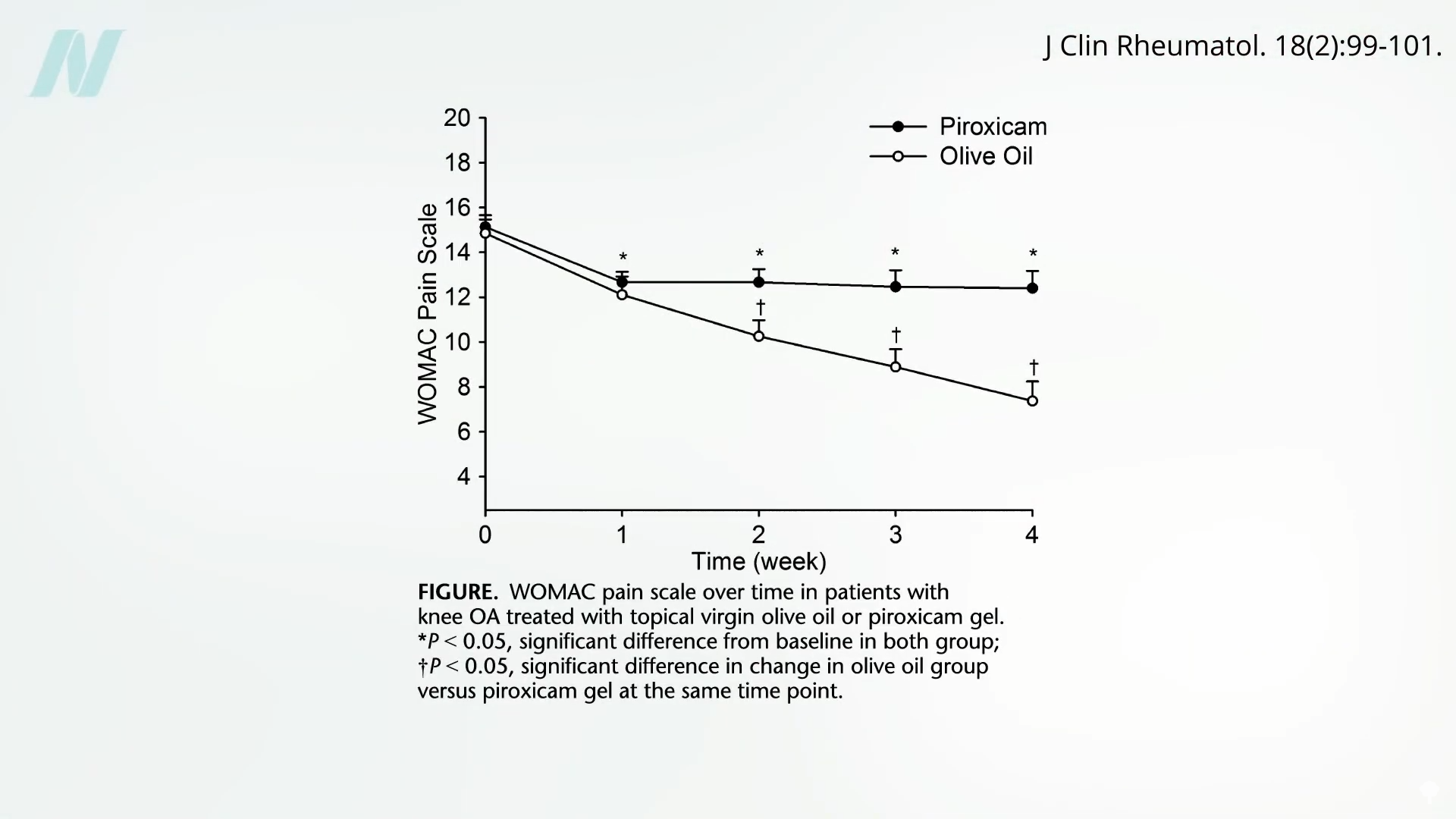
This particular study spanned only one month, leaving open the possibility that prolonged use of topical olive oil might yield even greater improvements over extended periods. Further research explored its utility in addressing morning stiffness and inflammatory pain in the fingers and knees among women diagnosed with rheumatoid arthritis. In this comprehensive evaluation, extra virgin olive oil was contrasted against both no treatment and the ibuprofen-type gel. The findings revealed that the olive oil group experienced a superior reduction in disease activity scores relative to the other interventions.
Key Insights on Natural Approaches to Arthritis Management
- The direct application of a modest quantity of extra virgin olive oil has been clinically proven to outperform standard ibuprofen-based gels in alleviating pain associated with both osteoarthritis and rheumatoid arthritis, presenting an economical and naturally derived option for symptom control.
- Although whole olives and certain olive extracts exhibit anti-inflammatory properties in preliminary studies, ingested extra virgin olive oil does not substantially mitigate inflammation or arthritis symptoms in humans, with some evidence indicating it is comparable to butter and inferior to coconut oil.
- Various foods with anti-inflammatory potential have been scrutinized, yet results vary widely. Strawberries, for example, successfully lowered inflammatory markers and provided clinically meaningful pain relief, whereas cherry juice and pomegranate juice, despite biochemical reductions, did not yield significant symptomatic improvements in arthritis patients.
These observations highlight the nuanced nature of dietary interventions for inflammatory joint conditions. While systemic consumption of olive oil may not offer robust benefits, its topical use emerges as a compelling, low-risk alternative worthy of further exploration and potential integration into arthritis care protocols. Researchers continue to investigate how natural compounds can complement or even surpass conventional pharmacological approaches, emphasizing the importance of evidence-based natural remedies in modern healthcare.









