Are you experiencing more issues with your digestive health as the temperatures plummet during the winter season?
This is a common reality, and it’s not something you’re making up in your mind.
The cold weather can take a serious toll on your gastrointestinal system, extending beyond just the excesses of holiday eating or heightened stress levels, although those factors certainly contribute significantly.
There are genuine biological mechanisms at play that explain why problems like bloating, constipation, and general abdominal unease tend to intensify as the mercury drops.
In this detailed guide, we’ll explore the underlying causes of these disruptions and provide practical, evidence-based strategies to counteract them effectively.

Your gastrointestinal tract is highly responsive to both external environmental conditions and internal bodily shifts, never functioning in complete isolation.
Winter conditions often converge to create an ideal scenario for various digestive disturbances to emerge.
Scientific investigations have revealed that the process of intestinal motility—the essential muscular contractions responsible for propelling food through the digestive pathway—naturally decelerates during the chillier periods of the year.
This phenomenon is supported by robust data, with multiple studies confirming distinct seasonal fluctuations in gut performance, where winter consistently registers the longest transit durations.
Consider the physiological response: in colder conditions, your body shifts its priorities to preserve core warmth, diverting blood circulation away from non-essential areas like the digestive organs to focus on thermoregulation. This reduced vascular supply to the gut results in suboptimal digestive processes.
Many individuals report this slowdown personally each winter, regardless of their best efforts to maintain healthy habits. Living in a place with harsh winters, like the Midwest, only amplifies the challenge.
Why Slow Motility Matters More Than You Think

Reduced intestinal motility goes far beyond mere occasional bouts of constipation, although that is undoubtedly one manifestation.
When contents linger excessively in the intestines, a cascade of complications arises that can profoundly impact overall health.
Key Consequences of Slow Motility
1. Increased Risk of Bacterial Overgrowth. Prolonged retention of food in the small intestine fosters an environment conducive to bacterial fermentation, producing excess gas, distension, and symptoms reminiscent of small intestinal bacterial overgrowth (SIBO).
2. Impaired Nutrient Uptake. The body relies on precise timing for optimal extraction of vitamins, minerals, and other essentials from food. Disruptions in transit timing can lead to deficiencies, even with a nutrient-dense diet.
It’s worth noting that the vast majority—around 90%—of nutrient absorption occurs specifically in the small intestine.
3. Heightened Toxin Reabsorption. Normally, the body efficiently encapsulates waste products and harmful substances for elimination. However, extended dwell time in the colon allows some of these toxins to diffuse back into the systemic circulation, exacerbating toxicity and inflammation.
Individuals already managing chronic gut conditions frequently notice a marked deterioration in symptoms during winter, underscoring the severity of these mechanisms.
The Stress Connection You Can’t Ignore
No discussion of winter gut challenges would be complete without addressing the pervasive role of stress.
Factors abound: festive season demands, diminished daylight hours, sunlight scarcity, seasonal mood disruptions, budgetary strains, and intricate family interactions.
Each of these triggers direct effects on the digestive system via the intricate gut-brain axis, a bidirectional communication highway between the central nervous system and the enteric nervous system.
Under stress, cortisol surges and the sympathetic nervous system dominates, initiating a fight-or-flight state that effectively pauses non-urgent functions like digestion. In survival mode, processing meals takes a backseat to perceived immediate threats.
Digestion becomes a low priority in such scenarios.
Prolonged stress exposure further disrupts gut physiology in several ways:
- Diminishes hydrochloric acid output in the stomach, crucial for breaking down proteins and killing pathogens.
- Suppresses the release of pancreatic and brush border enzymes needed for carbohydrate and fat metabolism.
- Shifts the composition of the gut microbiota toward less beneficial strains.
- Compromises the integrity of the intestinal lining, potentially leading to leaky gut.
Winter exacerbates these issues through additional deficiencies:
- Limited natural sunlight exposure, which influences serotonin production, mood stability, and microbial diversity.
- Reduced opportunities for physical activity, essential for promoting peristalsis and gut clearance.
- Fewer chances for outdoor time, depriving the microbiome of diverse environmental microbes.
- Disrupted sleep patterns, during which gut repair and regeneration predominantly occur.
Establishing a consistent nighttime routine can profoundly enhance sleep quality and, by extension, gut recovery.
Other Winter Factors Affecting Your Gut

Beyond motility and stress, several other seasonal elements conspire against digestive harmony.
1. Subtle Dehydration Risks. Colder air and indoor heating mask thirst signals, yet hydration demands remain constant. Insufficient fluid intake hardens stools and hampers motility, creating a vicious cycle.
2. Shifts in Eating Patterns. Cravings for hearty, warming dishes often mean heavier reliance on cooked foods, baked goods, and processed items, sidelining fresh produce and soluble fibers essential for smooth transit.
3. Sedentary Tendencies. The urge to hibernate reduces movement, yet even moderate exercise like brisk walking triggers the peristaltic waves necessary for efficient gut propulsion.
4. Vitamin D Deficiency Surge. Prolonged indoor confinement slashes sunlight-derived vitamin D synthesis, weakening mucosal barriers, immune vigilance, and microbial balance within the gut.
What Actually Helps (Beyond “Drink More Water”)
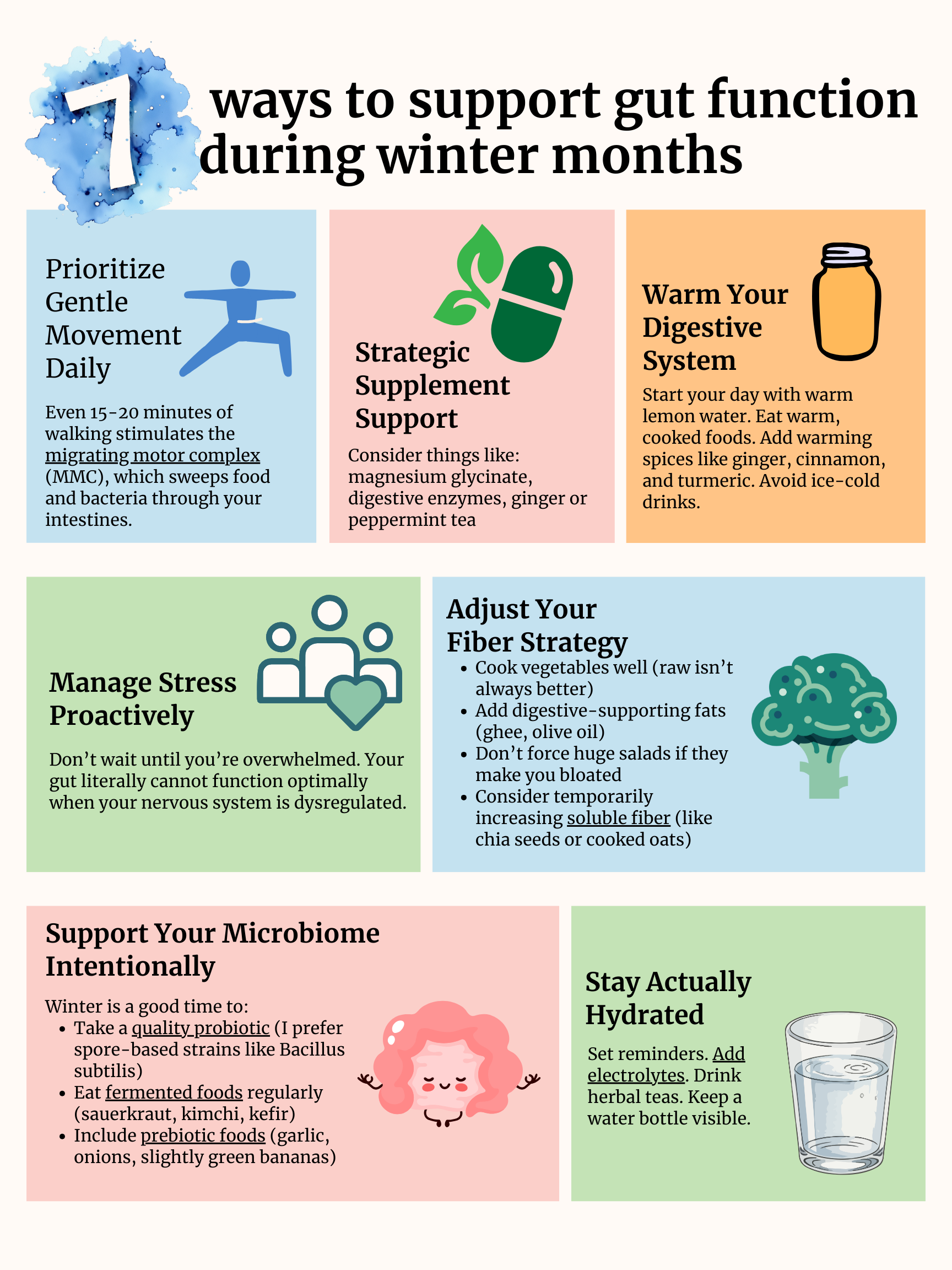
Drawing from personal experience and clinical insights, here are seven targeted approaches to bolster digestive resilience through the winter:
1. Prioritize Gentle Movement Daily. No need for grueling workouts—a modest 15-20 minute stroll activates the migrating motor complex (MMC), the housekeeping mechanism that clears residual debris and bacteria from the small intestine. Incorporating post-meal walks, even indoors, yields noticeable benefits. Complement this with a sustainable strength training regimen, such as 3-4 gym sessions weekly focused on resistance exercises, which enhance overall metabolic health.
2. Strategic Supplement Support. Magnesium glycinate taken in the evening aids relaxation, motility, and cortisol modulation. Pair it with specialized sleep aids for comprehensive restoration. Digestive enzymes with each meal offset stress-induced reductions in natural secretions. Herbal infusions like ginger or peppermint tea provide motility-boosting, anti-spasmodic effects backed by clinical trials. Immune-supportive formulas shine during peak respiratory season.
3. Warm Your Digestive System. Ancient healing traditions, including those from Chinese Medicine and Ayurveda, emphasize thermal support for digestion—a concept validated by modern science. Begin mornings with warm lemon water to stimulate gastric juices. Favor soups, stews, and spiced dishes incorporating ginger, cinnamon, and turmeric. Shun chilled beverages, as optimal enzyme function thrives in warmer environments, enhancing mucosal blood flow.
4. Manage Stress Proactively. Prevention trumps reaction: integrate brief breathwork or mindfulness sessions daily. Maintain circadian-aligned sleep schedules rigorously. Curate commitments to preserve energy. Morning red light therapy sessions recalibrate the nervous system, fostering parasympathetic dominance conducive to digestion.
A regulated autonomic nervous system is foundational for gut vitality.
5. Adjust Your Fiber Strategy. Seasonal produce like roots and brassicas demands robust digestion. Mitigate with thorough cooking, lubricating fats such as ghee or extra-virgin olive oil, and scaled-back raw intake if bloating ensues. Emphasize soluble fibers from sources like hydrated chia or oatmeal for gentler bulk formation during sluggish periods.
6. Stay Actually Hydrated. Combat forgetfulness with app reminders, electrolyte-enhanced waters, and aromatic herbal brews. Target intake equaling half your body weight in ounces daily, scaling up for exercise or dry heated air. Innovative bottles with purification and tracking features ensure compliance effortlessly.
7. Support Your Microbiome Intentionally. Microbial communities adapt to seasons, often diversifying less in winter. Counteract with spore-forming probiotics resilient to gastric acid, daily fermented condiments like sauerkraut or kefir, and prebiotic-rich alliums or resistant starches to cultivate a thriving ecosystem.
When to Seek Additional Support
Despite diligent implementation, persistent red flags warrant expert intervention:
- Severe constipation under three movements weekly.
- Intense, unrelenting bloating.
- Unexplained weight fluctuations.
- Visible or occult blood in stools.
- Chronic nausea interfering with daily life.
Winter may unmask latent conditions such as SIBO, intestinal methanogen overgrowth, or primary motility disorders, necessitating tailored diagnostics and therapies from functional or GI specialists.
The Bottom Line
Intensified gut symptoms in winter reflect adaptive responses to tangible climatic, hormonal, and lifestyle shifts—not personal shortcomings.
Empowering news: targeted interventions yield substantial relief. By fine-tuning motility promoters, stress buffers, hydration protocols, and microbial nurturing, you reclaim comfort and vitality amid the frost.
Perfection eludes us all; purposeful, incremental steps suffice for transformation.